Complications of diabetes – a disease affecting all organs
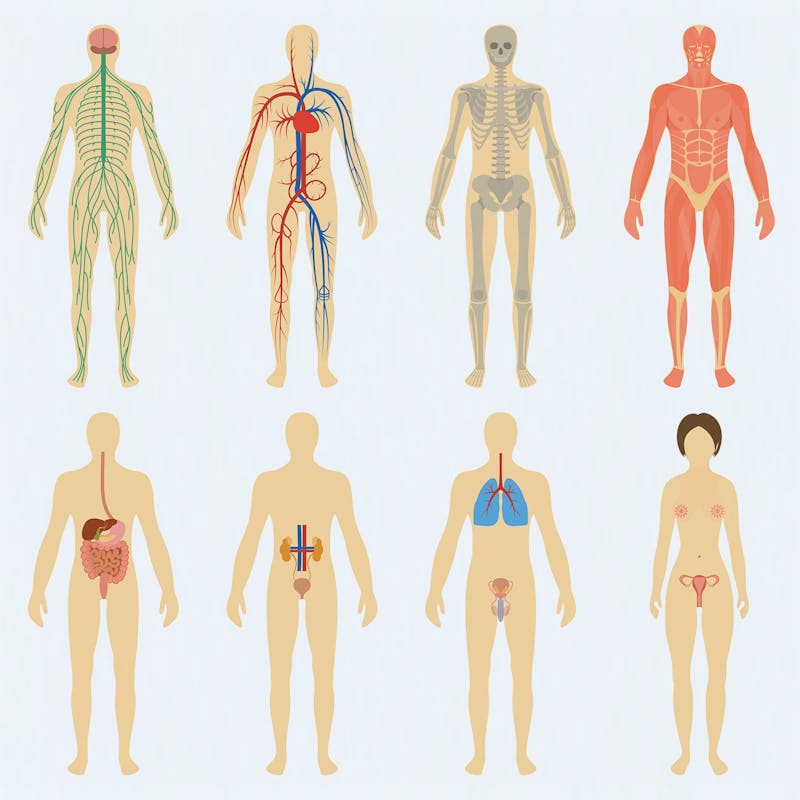
We’re treating people with type 2 diabetes completely wrong – and it’s harming every organ in their bodies.
Hyperglycemia (high blood sugar) may be the hallmark of diabetes, but does not cause most of the morbidity (the harm of the disease). Blood glucose is fairly easily controlled by medication, but this does not prevent the long-term complications. Despite blood glucose control, damage occurs to virtually every organ system.
It would be difficult to find a single organ system NOT affected by diabetes. These complications are generally classified as either microvascular (small blood vessels) or macrovascular (large blood vessels).
Certain organs, such as the eyes, kidneys and nerves are predominantly perfused by small blood vessels. Chronic damage to these small blood vessels causes failure of these organs. Damage to larger blood vessels results in narrowing called atherosclerotic plaque. When this plaque ruptures, it triggers an inflammatory reaction and blood clots that cause heart attacks and strokes. When blood flow is impaired to the legs, it may cause gangrene due to reduced circulation.
There are other complications do not fall neatly into this simple categorization. A variety of diabetic complications are not obviously caused by injured blood vessels. These would include skin conditions, fatty liver disease, infections, polycystic ovarian syndromes, Alzheimer’s disease and cancer.
Microvascular Complications
Retinopathy
Diabetes is the leading cause of new cases of blindness in the United States, according to the Center for Disease Control in 2011.
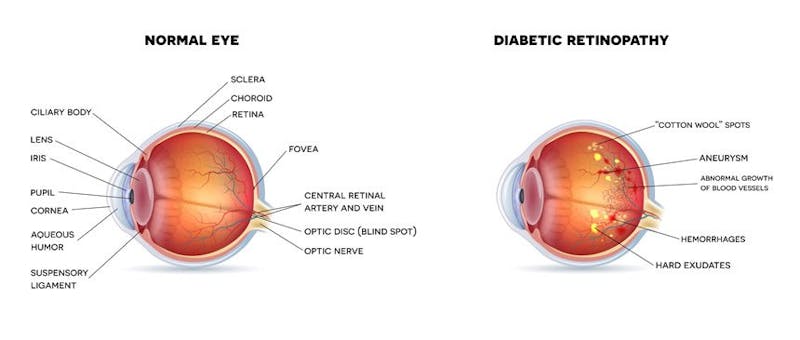
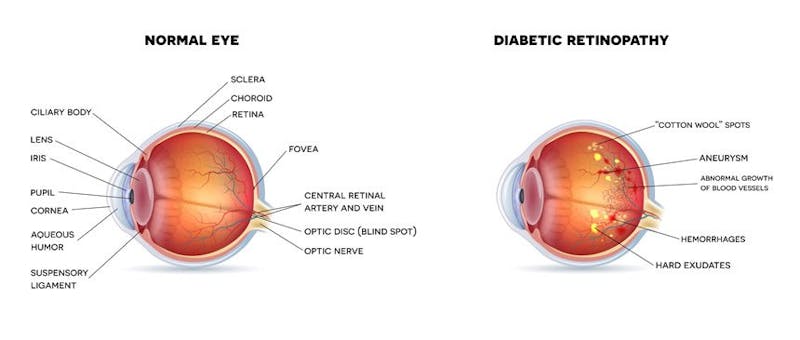
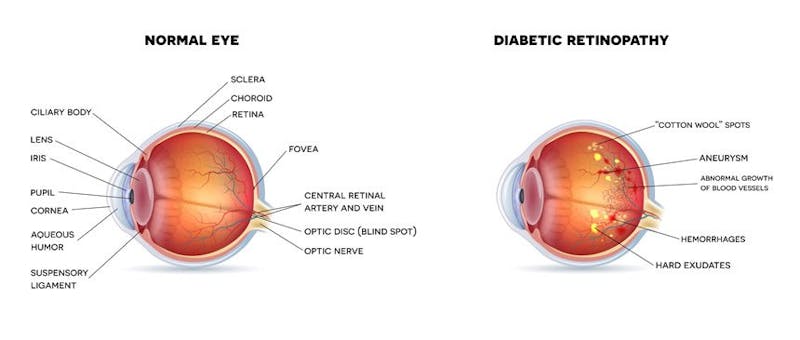
Eye disease, characteristically retinal damage (retinopathy) is one of the most frequent complications of diabetes. The retina is the light-sensitive nerve layer at the back of the eye that sends its ‘picture’ to the brain. Long standing diabetes weakens the small blood vessels in the back of the eye. Blood and other fluids leak out causing visual disturbances. This damage can be visualized with a standard ophthalmoscope during routine physical examinations. Bleeding into the retina appears as ‘dots’ and is therefore called ‘dot hemorrhages’. Lipid deposition at the margins of the bleeding is seen as ‘hard exudates’. The retina is the only place where this damage to the blood vessels can be directly visualized.
Over time, new blood vessels begin to form in the retina, but these are fragile and tend to break. This proliferation of new blood vessels leads to more bleeding inside the eye (vitreous hemorrhage) and/or formation of scar tissue. In severe cases, this scar tissue can lift the retina and pull away from its normal position. This detachment of the retina may lead to eventual blindness. Lasers are often used to prevent the formation of these new blood vessels.
Approximately 10,000 new cases of blindness in the United States are caused by diabetic retinopathy. The development of retinopathy depends upon the duration of diabetes as well as the severity of the disease. In type 1 diabetes, the majority of patients will have some degree of retinopathy within 20 years. In type 2 diabetes, retinopathy may actually develop up to 7 years prior to the diagnosis of diabetes itself.
Nephropathy
Diabetic kidney disease (nephropathy) is the leading cause of end stage renal failure (ESRD) in the United States accounting for 44% of all new cases in 2005. ESRD is defined as kidney failure requiring dialysis or transplantation, but many more are diagnosed with lesser degrees of chronic kidney disease. In the United States, more than 100,000 patients are diagnosed with chronic kidney disease annually. In 2005, it is estimated that care for kidney disease cost the United States $32 billion. The cost of this burden is enormous, both in financial and emotional terms.
One of the kidney’s major functions is to clean the blood of various toxins. As the kidney starts to fail, toxins build up in the blood leading to loss of appetite, weight loss, persistent nausea and vomiting and eventually to coma and death if untreated.
Dialysis is an artificial procedure to remove the accumulated toxins in the blood. It is only used when the kidneys has lost over 90% of their intrinsic function. The most common form of dialysis is hemodialysis where the blood is removed, cleaned through a dialysis machine, and then returned to the patient. Patients typically undergo dialysis three times a week for four hours each.



Neuropathy
Diabetic nerve damage (neuropathy) affects approximately 60-70% of patients with diabetes. There are many different types of diabetic nerve damage. Once again, the duration and severity of diabetes correlates with the occurrence of neuropathy.
The most common type of diabetic neuropathy affects the peripheral nerves. The feet are affected first, and then progressively, the hands and arms as well in a characteristic ‘stocking and glove’ distribution. Symptoms include:
- Tingling
- Numbness
- Burning
- Pain
Symptoms are often worse at night. The incessant pain of diabetic neuropathy is often one of the most debilitating aspects of this disease. Even powerful painkillers such as narcotic medications are often ineffective.
But the lack of symptoms does not mean that there is lack of nerve damage. Rather than pain, patients may experience complete numbness, with no sensation at all noted in the affected areas. Careful physical examination reveals decreased sensations of touch, vibration, temperature and loss of reflexes.
While loss of sensation seems innocuous, it is anything but. Pain protects against damaging trauma. Charcot foot is the progressive deformation caused by repeated trauma. Where most people would sensibly adjust their position when their feet start to hurt, patients with diabetes cannot feel these damaging episodes. Repeated over years, destruction of the joint ensues.
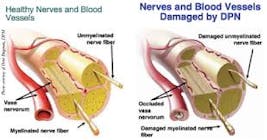
The autonomic nervous system controls our body functions that are not generally under conscious control, such as breathing, digestion, sweating, and heart rate. These nerves may also be damaged causing nausea, vomiting, constipation, diarrhea, anhidrosis (lack of sweating), bladder dysfunction, erectile dysfunction, and orthostatic hypotension (sudden, severe drop of blood pressure on standing). If cardiac innervation is affected, the risk of silent heart attacks and death is increased.
No current treatment reverses diabetic nerve damage. Drugs may help the symptoms of disease, but do not change its natural history. Ultimately, it can only be prevented.
Macrovascular disease
Atherosclerosis
Atherosclerosis is a disease of the arteries whereby plaques become deposited within the inner walls of the blood vessel. This causes the narrowing and hardening of arteries of all sizes. Diabetes greatly increases the risk of developing atherosclerosis. Atherosclerosis of the large blood vessels of the heart, brain, and legs are the standard cause of heart attacks, strokes and peripheral vascular disease respectively. Together, these diseases are known as cardiovascular diseases and are the main cause of death for people with diabetes.
The amount of death and disability resulting from cardiovascular diseases is an order of magnitude greater than from the microvascular disease. It is popularly imagined as cholesterol slowly clogging the arteries, much as sludge might build up in a pipe. However, this theory has long been known to be false.
Atherosclerosis results from injury to the endothelial lining of the artery. This allows infiltration of cholesterol particles into the lining of the artery wall causing inflammation. Smooth muscle proliferates and collagen accumulates in response to this injury, but this further narrows the vessel.
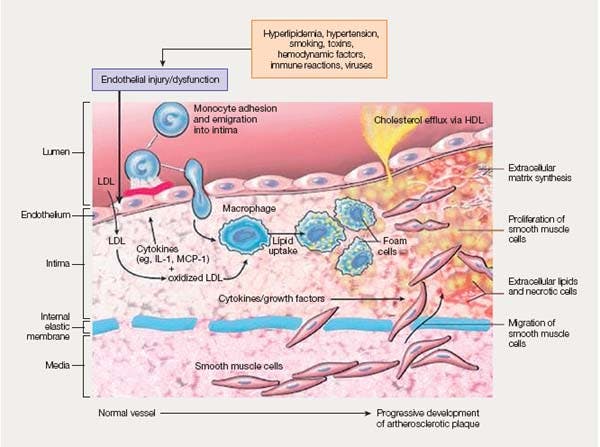
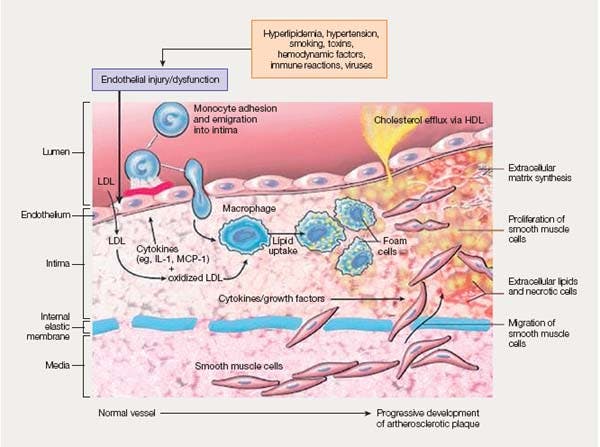
The end result is the development of the plaque, also known as the atheroma, covered with a fibrous cap. If this cap erodes, the underlying atheroma is exposed to the blood, triggering a blood clot. The sudden blockage of the artery by the clot prevents normal blood circulation and starves the downstream cells of oxygen. This causes heart attacks and strokes.
Atherosclerosis results from injury to the arterial wall rather than simply the buildup of cholesterol. Many factors contribute to this problem, including age, sex, smoking, physical activity, family history, stress, and high blood pressure. However, diabetes is one of the greatest risk factors for atherosclerosis.
Heart Disease
Heart disease is the most well-recognized and feared complication of diabetes. The presence of diabetes increases the risk of cardiovascular disease at least two to four times higher. Complications develop at a younger age. According to the American Heart Association, at least sixty eight percent of people with diabetes aged 65 or older will die of heart disease compared to sixteen percent who will die of stroke. Because more than eighty percent of people with diabetes will die of CV disease, reducing macrovascular disease is of primary importance, even above those of microvascular concerns.
The Framingham studies of the 1970s established the firm association between heart disease and diabetes. The risk is so high that having diabetes is considered the equivalent of having had a previous heart attack. Patients with diabetes have over three times the risk of heart attack compared to patients without diabetes. Over the past three decades, there have been significant improvements in treatment, but the gains for patients with diabetes have lagged far behind. While overall death rates for men without diabetes have decreased by 36.4%, it only decreased 13.1% for men with diabetes. In women without diabetes, death rate decreased by 27% but increased 23% in women with.
Stroke
The devastating impact of stroke cannot be underestimated. In the United States, it is the third leading cause of death and the biggest contributor to disability. Diabetes is a strong independent risk factor in stroke, increasing risk by as much as 150-400%. It is estimated that approximately ¼ of all new strokes occur in patients with diabetes. The risk of stroke rises 3% for each year of diabetes. The prognosis of stroke in patients with diabetes is also worse than those without.
Peripheral Vascular Disease
Peripheral vascular disease (PVD) is caused by the blockage of blood vessels going to the lower extremities. It may happen in the hands and arms, too, but this is uncommon. The progressive narrowing of the blood vessels starves the legs of much-needed oxygen carrying hemoglobin.
Intermittent claudication, pain or cramping that appears with walking and relieved by rest is the most common symptom. As circulation worsens, pain may appear at rest and is especially common at night. Diabetic foot ulcers may occur and progress to gangrene in severe cases. At this point, amputation is often necessary.
Diabetes, along with smoking, is the strongest risk factor for PVD. Over a 5 years period, approximately 27% of patients will have progressive disease and amputation will occur in 4%. PVD significantly reduces mobility leading to long-term disability. Intermittent claudication results in reduced mobility. Patients with gangrene and those requiring amputation may never walk again. This may result in a ‘cycle of disability’ with progressive deconditioning of muscles. Severe unrelenting pain impairs quality of life.
Other complications
Cancer
Many common cancers are related to type 2 diabetes. This includes breast, stomach, colorectal, kidney and endometrial cancers. In addition, survival of cancer patients with pre-existing diabetes is far worse than those without diabetes.
Skin and Nails
Patients with type 2 diabetes commonly manifest some form of skin disease. Acanthosis nigricans is a gray-black, velvety, thickening of the skin, particularly around the neck and in body folds. High insulin levels stimulate the growth of keratinocytes to produce the thickened skin.
Diabetic dermopathy, also called shin spots, are often found on the lower extremities as hyperpigemented, finely scaled lesions. Skin tags are soft protrusions of skin often found on the eyelids, neck and under the arms. Over twenty-five percent of patients with skin tags have diabetes.
Nail problems are common in patients with diabetes, particularly fungal infections. Nails become discolored to a yellowy-brown color, thicken and separate from the nail bed (onycholysis).
Infections
In general, patients with diabetes are more prone to all types of infections, which tend to be more serious than those without diabetes. Simple bladder infections are increased, but also the more serious kidney infection (pyelonephritis). This risk is increased 4-5 fold in patients with diabetes and tends to involve both kidneys. Complications such as abscess formation and renal papillary necrosis are also more common in patients with diabetes.
All types of fungal infections are more common in patients with diabetes. This includes oral thrush, vulvovaginal yeast infections, fungal infections of the nail, and athlete’s foot.
Diabetic Foot Ulcers



Despite adequate blood glucose control, 15 % of all patients with diabetes will develop non-healing foot wounds during their lifetime. Patients with diabetes have a 15-fold increased risk of lower-limb amputation, and account for over 50% of the amputations done in the United States excluding accidents. The financial cost of these diabetic foot problems cannot be underestimated. It is estimated that each case costs upwards of $25,000 to treat.
Erectile Dysfunction
Community based population studies of aging males age 39-70 years found that the prevalence of impotence ranges between ten and fifty percent. Diabetes is a key risk factor, increasing the risk is more than three fold. Erectile dysfunction affects patients with diabetes at a younger age than those without diabetes.
Fatty Liver
Non-alcoholic fatty liver disease (NAFLD) is the storage and accumulation of excess fat in the form of triglycerides exceeding 5% of the total weight of the liver. When this excess fat causes damage to the liver tissue, detectable on standard blood tests, it is called non-alcoholic steatohepatitis (NASH). This is not a trivial issue as NASH is expected to be the leading cause of liver cirrhosis in North America.
In type 1 diabetes, there is a very low incidence of fatty liver disease. By contrast, the incidence is very high in type 2 diabetes, often estimated at upwards of 75%.
Polycystic Ovarian Syndrome
Polycystic ovarian syndrome (PCOS) is characterized by irregular menstrual cycles, evidence of excessive testosterone, and ultrasound findings of cysts. PCOS patients share many of the same characteristics as patients with type 2 diabetes, including obesity, high blood pressure, high cholesterol, and insulin resistance. It is commonly considered part of the metabolic syndrome and an earlier manifestation of the insulin resistance that is characteristic of type 2 diabetes.
Alzheimer’s Disease
Alzheimer’s disease is a chronic progressive neurodegenerative disease that causes memory loss, personality changes, and cognitive problems. It is the most common form of dementia totaling 60-70% of all cases. The links between Alzheimer’s disease and diabetes continue to grow stronger. Many have argued that Alzheimer’s disease can be called ‘type 3 diabetes’ given the central role of insulin resistance in the brain.
Summary
Every single organ system is affected by diabetes. Diabetes has the unique malignant potential to devastate our entire body. But why? Virtually every other disease is limited to a single organ system. Diabetes affects every organ in multiple ways. It is the leading cause of blindness. It is the leading cause of kidney failure. It is the leading cause of heart disease. It is the leading cause of stroke. It is the leading cause of amputations. It is the leading cause of dementia. It is the leading cause of infertility. It is the leading cause of nerve damage.
Why are these problems getting worse, not better, even centuries after the disease was first described? We assume that complications arise due to damage caused by hyperglycemia. But as we develop newer, better medications to control hyperglycemia, why do complications rates not improve? We expect that over time, as our understanding of diabetes increases, that the rates should decrease. But they don’t. We are in the midst of a worldwide epidemic of type 2 diabetes. Worse, rates are accelerating, not decelerating. We must face the cold and hard-as-steel fact that our current path leads to failure.
If the situation is getting worse, then the only logical explanation is that our understanding and treatment of type 2 diabetes is fundamentally flawed. We may be running hard, but in the wrong direction. Even a cursory glance at our treatment paradigm reveals the problem. The unspoken premise of our current treatment paradigm is that the toxicity of type 2 diabetes develops only from high blood glucose. Therefore, drug treatments are all directed towards lowering blood glucose.
However, we also know that insulin resistance causes the hyperglycemia in type 2 diabetes. If our drugs do not correct the underlying insulin resistance, then they only treat the symptoms of hyperglycemia. The underlying disease (high insulin resistance) remains completely untreated. We have no hope of eradicating this disease without addressing the root cause.
—
Jason Fung
Earlier
Why High Blood Sugar Is Not the Main Problem
The Futility of Blood Sugar Lowering by Medications in T2D
A New Paradigm of Insulin Resistance
More
If you want to learn more about how to reverse your type 2 diabetes on low carb, or troubleshoot if you run into any problem, check out our full guide below. Alternatively choose the quick start guide with only the two most effective simple steps!
Popular videos about diabetes
- MEMBERS ONLY
![Part 8 of Dr. Jason Fung's diabetes course]()
Earlier with Dr. Jason Fung
How to Renew Your Body: Fasting and Autophagy
How Much Protein Should You Eat?
The Common Currency in Our Bodies Is Not Calories – Guess What It Is?
Why the First Law of Thermodynamics Is Utterly Irrelevant
How to Fix Your Broken Metabolism by Doing the Exact Opposite
More with Dr. Fung
Dr. Fung has his own blog at intensivedietarymanagement.com. He is also active on Twitter.
His book The Obesity Code is available on Amazon.