What is normal blood pressure?
Optimal, ideal, excellent, healthy: isn’t that how we’d all love our blood pressure to be? Normal, healthy blood pressure is one of the most important measurements for long-term health and can help prevent or reduce many health problems.
This guide will help explain optimal blood pressure numbers, some factors that can influence normal results, and ways to keep readings in that ideal, healthy range.
1. What is blood pressure?
To understand normal or healthy blood pressure, it helps to understand blood pressure itself.
When our heart contracts (pumps, or beats), it pushes blood out of the chambers of the heart. This contraction exerts a force on the body’s arteries that deliver blood to the tissues. This force is called the systolic blood pressure, which is the top number in your blood pressure measurement.
When the heart relaxes, blood refills the chambers of the heart. This relaxation creates another pressure in the arteries at rest. Called the diastolic blood pressure, this is the bottom number in your blood pressure measurement.
It is common to forget which is the systolic and which is the diastolic number. Here is a simple trick to remember: think of S — Sky — for the top; and D — Dirt — for the bottom.
A normal blood pressure is any systolic number under 120 and any diastolic number under 80, measured in millimetres of mercury, or mm Hg.1 This is written as 120/80 or spoken as “120 over 80”. We will get into more discussion shortly about the range of readings that indicate optimal or healthy blood pressure.
2. Why is normal blood pressure important?
Just like water flowing through a garden hose, blood flowing through your blood vessels needs to have enough healthy pressure to circulate throughout your body to deliver oxygen-rich blood and nutrients to every cell, from the tip of your toes to the top of your head.
If blood pressure rises too high, it is called hypertension. Just as a garden hose under too much pressure may damage the walls of the hose, and the stream of water can be too strong when blasted on delicate plants, blood flowing through our blood vessels under too much pressure can weaken and damage blood vessel walls, or damage delicate organ structures and tissues that receive the high-pressure flow.
Blood vessel damage from high blood pressure can predispose us to strokes, heart attacks, heart disease, kidney damage, eye damage and even dementia.2 The longer blood pressure stays high, the more damage it can cause.
While less commonly of concern, when blood pressure is too low — called hypotension — blood may not circulate adequately, causing dizziness and fainting, especially when standing up from a sitting or lying position. Weakness and fatigue may also be common.
That is why blood pressure in the normal, healthy range is so important. The right level of pressure allows blood to flow throughout the body’s vessels, delivering oxygen and nutrients, getting to all the cells unimpeded, but not doing any damage to tissues in the process.
3. How is blood pressure measured?
To get an accurate reading, it is important that blood pressure be measured properly.3 You should be sitting quietly, both feet flat on the floor. The arm in which your pressure is being measured should be supported at the level of your heart.
For a manual measurement, a cuff that is properly sized to your arm is inflated until blood flow stops.4 Pressure is slowly released until the very first sound of blood flow is heard. That moment is the top (systolic) number. Cuff pressure continues to be released until no more sound is heard. This point is the lower (diastolic) number.
These days accurate machines can do this measurement automatically. Many doctors now have these machines in their offices. You will also find them in some pharmacies, gyms, and available as home monitors.
Getting accurate measurements
Sometimes one blood pressure measurement is enough. However, to get really accurate measurements, doctors may take — or have a machine take — a number of readings over a 10 to 30-minute period.5 For home measurements, it is recommended that you take three consecutive measurements and record the average.
If there is any doubt about the accuracy of your readings, you may even be sent home with an ambulatory blood pressure monitor that you wear for 24 hours. It will take measurements as you go about your day and also measure blood pressure as you sleep, exercise or do other physical activities.6 This 24-hour measurement can confirm whether your blood pressure is normal or not and mitigate the risk that you may be treated unnecessarily.
It is a good idea to keep track of your typical blood pressure readings so you know whether your blood pressure is stable, getting worse, or getting better over time. Many people have no idea whether they have normal blood pressure or how their numbers may be changing. Recording your results is as easy as keeping track on a pad of paper kept next to your cuff, or creating a spread sheet on your computer. The key is having the numbers handy to go back and reference.
A campaign in both the UK and North America urges “Know your numbers” so that you are aware when you have normal, healthy blood pressure and when you might be trending to unhealthy higher levels.
4. Blood pressure graph – what the numbers mean
Here is a visual graph of all the ranges of various blood pressures. The green section of the graph displays the range of normal blood pressures.
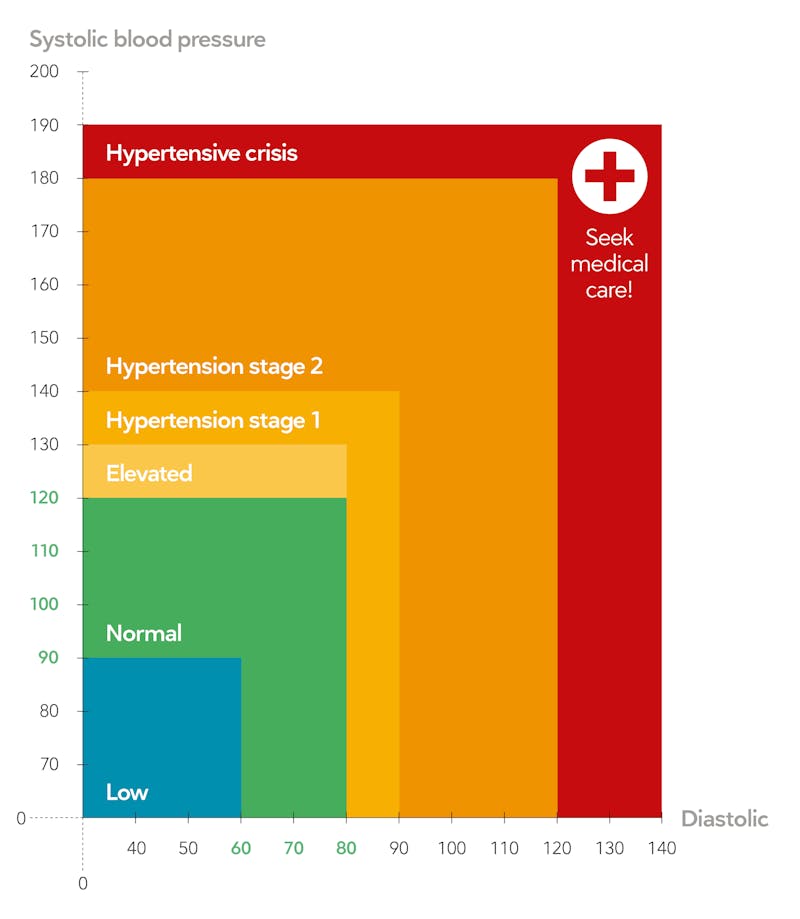
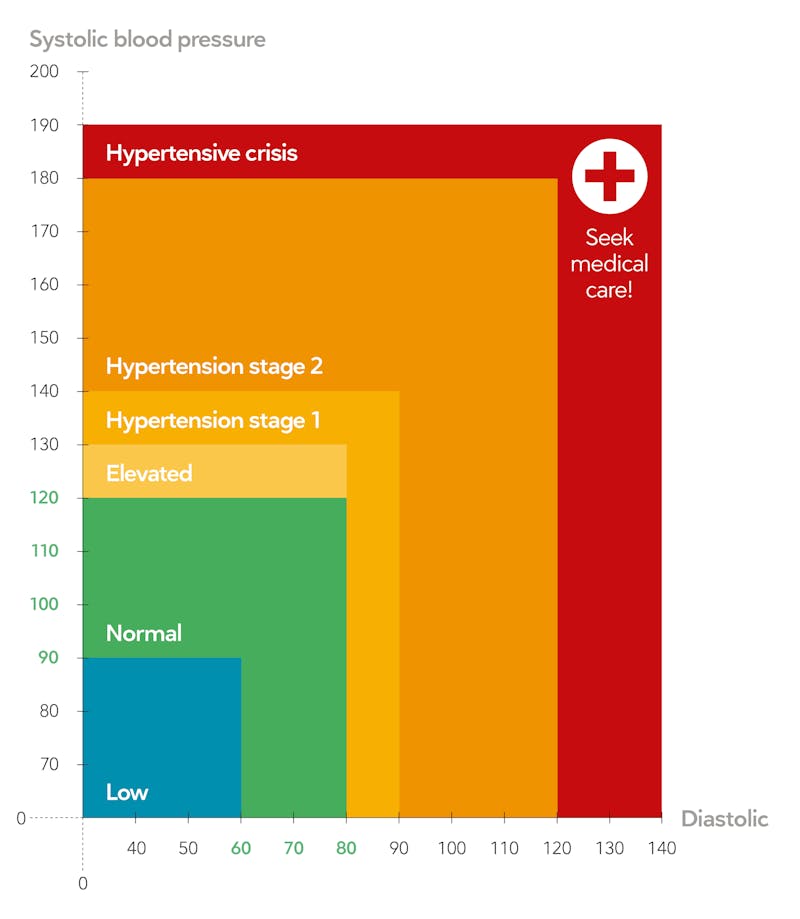
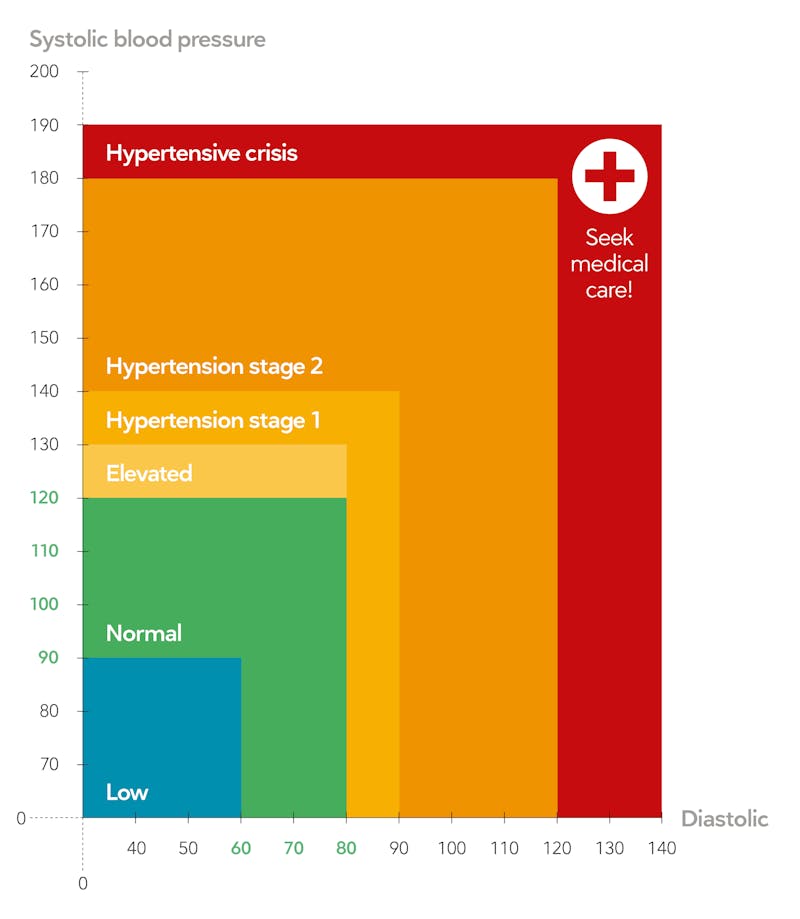
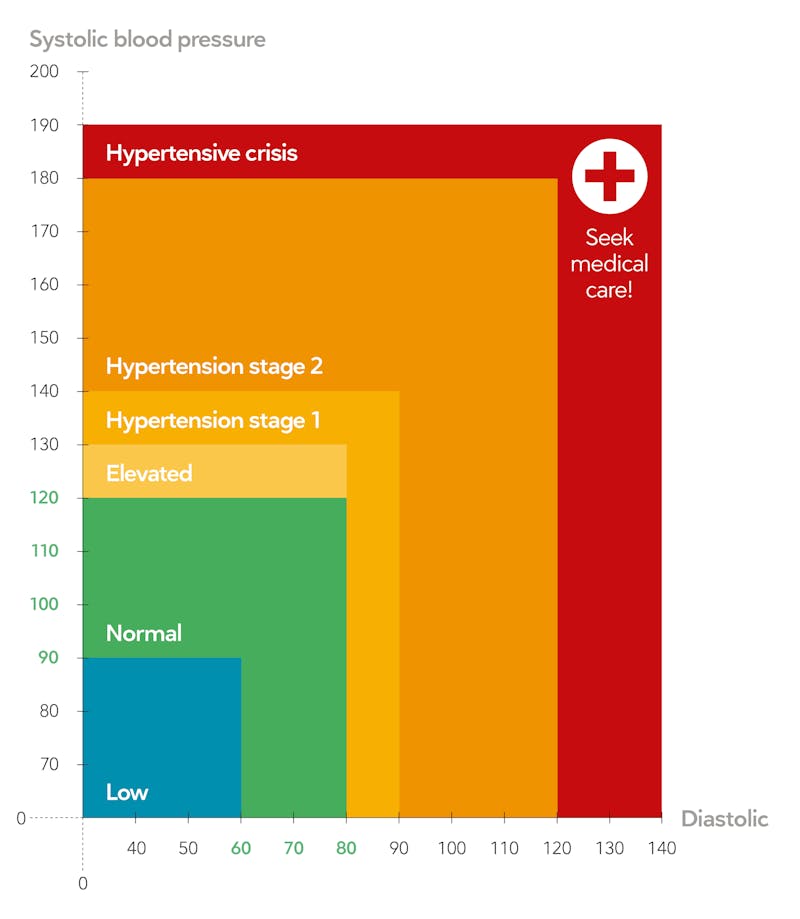
Keep in mind that blood pressure varies throughout the day; it won’t be the same every time you check it. What matters most is the average blood pressure for the day.
Over time you may detect patterns or situations that make your blood pressure readings slightly higher or lower, such as sleep quality, stress, and activities. Even dietary choices, such as salt consumption for the 25% of individuals with normal blood pressure who are salt sensitive, can affect your readings.8
Note: If your blood pressure is ever higher than 180/120 it is a hypertensive crisis. Please call your doctor or go to the Emergency Department immediately.
If your blood pressure falls in the stage 1 (yellow) or stage 2 (orange) category for hypertension, please see the following guide and contact your physician for guidance.


How to normalize your blood pressure
Guide Elevated blood pressure is a common health issue today, but you can improve your blood pressure using simple lifestyle changes.
5. How normal blood pressure changes with age
As we age, our blood vessels naturally stiffen. This causes the systolic blood pressure to increase in those over the age of 65 while the diastolic pressure often does not increase.9 For that reason, a normal healthy blood pressure in older adults can be up to and include a 140 systolic number with a relatively normal diastolic number between 60 and 80 — with no need for any treatment.10 This means normal — untreated — blood pressure for an elderly individual can be many points higher than for a younger person.
In fact, in some countries, health guidelines recommend that no blood pressure treatment be given to an individual over the age of 65 until the systolic pressure is at least 150, or even as high as 160, to balance the risk and benefits of any blood pressure lowering medications.11
That’s because reducing the blood pressure of elderly individuals with medications too intensely can be associated with adverse side effects, such as dizzy spells, low blood pressure, and the risks of falls when getting up quickly. However, for others, especially those at higher risk of cardiovascular disease, reducing blood pressure below 140 may help prevent a future heart attack or stroke.
The US based guidelines now recommend treating blood pressure to a goal of less than 130/80 even in the elderly. This change was based mostly off of a trial that showed a small benefit with more aggressive treatment.12 However, the trial also showed a significant increase in concerning side effects. That means the pros and cons of treating or not treating must be carefully weighed. So “normal” or optimal blood pressure in the context of an elderly person must be individualized.
Again, the best advice is to know your blood pressure numbers and how they are changing. Then work with your doctor to decide what blood pressure target is normal, optimal and healthy for you as you age.13
6. Inaccurate normal blood pressure results
Sometimes when a blood pressure is taken by a medical professional the result may not truly reflect your regular day-to-day blood pressure. This can happen with two conditions:
- White coat hypertension: This reaction has been well-known for at least a century and impacts about 15% of people. Outside the doctor’s office, the individual’s blood pressure is in the normal range but when the doctor goes to take the blood pressure measurement, the patient’s blood pressure suddenly spikes into the hypertensive range.14 It is thought to be a stress or anxiety response, but individuals who have this reaction may have little or no control over it even if they consciously try to relax.
If your blood pressure is in the normal range when you take it at an automatic machine in a pharmacy, gym or with a home monitor, be sure to tell your doctor about these normal readings, especially if your blood pressure is higher in the office. Regular home blood pressure measurements or a 24-hour ambulatory blood pressure monitor can establish that your blood pressure is actually normal. This will prevent a misdiagnosis and prevent the unnecessary treatment with medication.Research has shown, however, that individuals with white coat hypertension may eventually see their normal blood pressures rise into the true hypertensive range and be at higher risk of future blood sugar problems and cardiovascular disease.15 Again, know your numbers and track your trends.
- Masked hypertension: This condition is the exact opposite of white coat hypertension. In the doctor’s office, the individual’s blood pressure measurement is in the normal, healthy range, but in other situations, especially at night, it rises into the hypertensive range.16
Unlike white coat hypertension, the awareness of the prevalence of masked hypertension is relatively new — largely discovered through the use of 24-hour ambulatory blood pressure monitors and wider use of automatic home blood pressure machines.
Masked hypertension is estimated to impact about 9% of Europeans and 12% of US people, with African-Americans affected at higher rates of about 16%.17 It is also found in higher rates in individuals who have any of the following health issues: a high consumption of alcohol or tobacco; high work or home mental stress; obesity; low exercise tolerance; metabolic syndrome; type 2 diabetes; and sleep apnea.18
If your blood pressure is normal in office readings but you have risk factors or suspicion for masked hypertension, a 24-hour ambulatory blood pressure monitor will help confirm or dismiss the diagnosis.




7. What else might raise blood pressure?
A number of common drugs, supplements and compounds can raise what is essentially normal blood pressure out of the normal range. Stopping these substances can often return blood pressure to optimal levels. These substances include:
- Oral contraceptives and hormone replacement therapy, especially with higher estrogen levels.19
- Oral decongestants found in some cold and allergy medications.20
- Non-steroidal anti-inflammatories (NSAIDs) for pain relief and inflammation.21
- Herbal supplements including St. John’s Wort, ginseng, ginkgo, blue kohosh.22
- A compound in licorice root called glycyrrhizin, which is found in licorice-flavoured herbal teas, candies, lozenges, herbal remedies and is very potent in raising blood pressure, prompting a number of case studies and a warning from the US Food and Drug Agency.23
- Alcohol dependence, especially if consumed in larger quantities on a daily basis.24
- Cocaine, methamphetamines and other recreational stimulant drugs.25
- Tobacco use, particularly smokeless (chewing) tobacco.26
If you are taking any of these items regularly and receive a high blood pressure reading, stopping their use may help your blood pressure return to the normal range.
Some substances, not listed, may also increase blood pressure or may interact with other medications to raise blood pressure. If your blood pressure unexpectedly increases out of normal ranges it is a good idea to review with your doctor or pharmacist all medications, supplements, and other products you are using that may have contributed to this rise.
8. Keeping your blood pressure optimal
A number of lifestyle habits are very powerful to keep your blood pressure healthy and optimal. If you currently have normal blood pressure, paying attention to these habits will likely keep your blood pressure healthy and normal for many years to come.27
If your blood pressure is trending higher or if you are already being treated for hypertension, adopting or focusing on these lifestyle habits may stop the rise or bring it back into normal range, either preventing the need for medication or enabling the removal of medications.
- Keep a healthy weight or lose weight — adopting a low-carb diet can be a great way to lose weight and help keep blood pressure normal.28
- Reduce or eliminate added sugars, especially in processed foods and sugar-sweetened beverages. Some experts now think sugar, especially fructose, may be more influential on blood pressure than salt.29
- Exercise regularly.
- Keep your alcohol consumption low or moderate.
- Quit or never start smoking or using smokeless tobacco.
- Add meditation and relaxation routines into your life.
- Explore whether you are salt sensitive. About 25% of people with normal blood pressure find their blood pressure levels may be influenced by the salt they eat in their diet.30
You can read more in our guide on how to normalize your blood pressure naturally.
9. Summary
Keeping your blood pressure in normal ranges of below 130/80 is one of the best things you can do for your long-term health.
Fortunately, blood pressure levels are very responsive to healthy lifestyle changes. A low-carbohydrate ketogenic diet is an especially effective way to normalize your blood pressure naturally. Check out these other Diet Doctor comprehensive guides below.
Heart disease
This definition is based on the 2017 update by the ACC, AHA, and other medical societies.
Hypertension 2018: 2017 ACC-AHA-AAPA-ABC-ACPM-AGS-APhA-ASH-ASPC-NMA-PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines[overview article; ungraded]
However, not all societies agree with the definition. In 2020, the International Society for Hypertension defined normal blood pressure as anything under 130/85.
Hypertension 2020: 2020 International Society of Hypertension Global Hypertension Practice Guidelines[overview article; ungraded]
↩Hypertension 2015: Higher blood pressure as a risk factor for diseases other than stroke and ischemic heart disease [overview article; ungraded] ↩
Journal of American College of Cardiology 2017: Accuracy of cuff-measured blood pressure: Systematic reviews and meta-analyses [strong evidence] ↩
American Journal of Hypertension 2002: Arm cuff in the measurement of blood pressure [overview; ungraded] ↩
Annals of Family Medicine 2017: Thirty-minute office blood pressure monitoring in primary care [case series; weak evidence] ↩
Current Atherosclerosis Reports 2013: Ambulatory blood pressure improves prediction of cardiovascular risk: implications for better antihypertensive management [overview; ungraded]
American Journal of Medicine 2015: Ambulatory blood pressure monitoring in clinical practice: a review [overview; ungraded] ↩
American College of Cardiology: 2017 guideline for high blood pressure in adults [overview article; ungraded evidence] ↩
Many promote low salt diets for all out of concern that salt can dangerously raise blood pressure. However, research suggests this is only the case for around 25% of the population, and therefore likely not a concern for the rest.
Current Opinion in Nephrology and Hypertension 2012: Mechanisms and consequences of salt sensitivity and dietary salt intake [overview article; ungraded] ↩
Family Practice Essentials 2018: Hypertension update: Older adults [overview; ungraded] ↩
This is controversial as there are differing guidelines among different countries. We will highlight some of these differences in the text that follows. ↩
Journal of Internal Medicine 2015: Benefits and risks of antihypertensive medications in the elderly [overview; ungraded]
European Heart Journal Supplement 2019: Hypertension in the elderly: which are the blood pressure threshold values? [expert review, ungraded] ↩
The New England Journal of Medicine 2015: A randomized trial of intensive versus standard blood-pressure control [randomized controlled trial; moderate evidence] ↩
Journal of the American College of Cardiology 2017: Outcomes of intensive blood pressure lowering in older hypertensive patients [meta-analysis of RCTs; strong evidence] ↩
Clinical and Experimental Pharmacology and Physiology 2014: White-coat hypertension [overview; ungraded] ↩
Journal of Hypertension 2016: White-coat hypertension and cardiovascular events: a meta-analysis [meta analysis of observational studies, very weak evidence] ↩
European Heart Journal 2017: Masked hypertension: understanding its complexity[overview article; ungraded] ↩
Current Hypertension Reports 2017: An update on masked hypertension [overview article; ungraded] ↩
American Heart Association Hypertension 2015: Masked hypertension — Phenomenon of measurement [overview; ungraded] ↩
Uptodate 2018: Effect of hormonal contraceptives and postmenopausal hormone therapy on blood pressure [overview; ungraded] ↩
Archives of Internal Medicine 2005: Effect of oral pseudoephedrine on blood pressure and heart rate [meta-analysis of RCTs; strong evidence] ↩
Journal of Clinical Hypertension 2007: Drug interactions and drugs that affect blood pressure [overview; ungraded] ↩
Plastic Reconstructive Surgery 2013: Herbal products that may contribute to hypertension [overview; ungraded]
American Journal of Hypertension 2001: Herbs and supplements in the hypertension clinic [overview; ungraded] ↩
British Medical Journal Case Reports 2015: Hypertension induced by liquorice tea [Case report and review of the literature; weak evidence] ↩
World Journal of Cardiology 2014: Alcohol-induced hypertension — Mechanisms and prevention [overview; ungraded] ↩
Pharmacological Research 1999: Cocaine-induced hypertension [mechanistic study; ungraded]
Heart, Lung and Circulation 2016: The cardiac complications of methamphetamines [overview; ungraded] ↩
Southern Medical Journal 1995: Does smokeless tobacco cause hypertension? [overview; ungraded] ↩
Journal of Hypertension and Management 2018: Lifestyle and hypertension: An evidence-based review [overview article; ungraded evidence] ↩
Obesity Reviews 2009: Systematic review of randomized controlled trials of low-carbohydrate vs. low-fat/low-calorie diets in the management of obesity and its comorbidities [strong evidence] ↩
Open Heart 2014: The wrong white crystals: not salt but sugar as aetiological in hypertension and cardiometabolic disease [overview; ungraded] ↩
Current Opinion in Nephrology and Hypertension 2012: Mechanisms and consequences of salt sensitivity and dietary salt intake [overview article; ungraded] ↩