What is a CGM — and is it right for you?
If you have type 1 or 2 diabetes, you know how vital it can be to monitor and control your blood glucose. But, even if you don’t have either condition, keeping track of your blood glucose levels may still be a smart idea for many people.
Why? Increasing blood sugar and declining metabolic health are associated with a higher risk of multiple diseases, including cancer, heart disease, dementia, and even early death.1
The good news is, using a continuous glucose monitor (CGM) can help. In the U.S. and some other jurisdictions, you’ll need to talk to your doctor about getting one of these, since CGMs require prescriptions.2 However others, like Canada, do not require prescriptions. You may need to pay upward of $80 for a monitor, but it may be worth it since CGM data can help you take action toward improving your metabolic health and reducing your risk of chronic diseases.
Here’s all you need to know about CGMs and how to use them to improve your metabolic health.

Summary
- CGMs allow you to track your blood sugar all day long — including after eating — which provides greater insight than simply checking fasting levels.
- CGMs give you real-time data, allowing you to make moment-to-moment decisions about food and lifestyle.
- Because traditional blood work is limited to fasting blood sugar and hemoglobin A1c (HbA1c), current definitions of “normal” blood sugar miss many people who may be at risk for metabolic dysfunction. CGMs address that.
- CGMs are the best tools for measuring your individualized glucose response — a powerful way to learn more about your metabolic health and possibly lower your risk of many chronic diseases.
Start your FREE 7-day trial!
Get instant access to healthy low-carb and keto meal plans, fast and easy recipes, weight loss advice from medical experts, and so much more. A healthier life starts now with your free trial!
Start FREE trial!
1. What is a CGM?




A CGM is a small medical device that monitors your blood sugar in real-time.
Most devices go on your abdomen or upper triceps and stay in place for 7 to 14 days. An adhesive patch keeps the CGM attached, and it sends blood sugar readings to a proprietary receiver or — more commonly nowadays — an app on your phone.
Here’s what’s so amazing: when wearing a CGM, the only part that goes “inside” your body is a thin microfilament that you don’t even feel! It sits in what is called the “interstitial space” under your skin.
This means it makes contact with the fluid surrounding your cells and is not in a blood vessel. Not being in the blood vessel keeps any risk for bleeding or infection down to almost zero.
Doctors most commonly prescribe CGMs for people with type 1 or 2 diabetes who take insulin. Having immediate blood sugar feedback has revolutionized people’s ability to dose mealtime insulin accurately, leading to more time in a healthy range, fewer life-threatening hypoglycemic episodes, and less frequent undetected rises in blood sugar.3
More recently, CGMs are becoming recognized as a general tool for improving metabolic health. My own patients, for example, have enjoyed having a real-time way of tracking their progress and seeing immediate effects of their lifestyle changes— regardless of whether they have diabetes.4
Could wearing a CGM help you?
2. Is a CGM right for you?




In general, many people might benefit from wearing a CGM, but there are certain instances where it might not be right for you. Here’s how to know whether using a CGM might be worth a try.
Who should consider a CGM:
- You have type 1 or type 2 diabetes and want to keep your blood sugar within an ideal range. Talk to your doctor to make sure you can do this safely.
- You have metabolic syndrome and want accurate, real-time blood sugar monitoring.
- You want to “optimize” your metabolic health through lifestyle interventions.
- As part of your weight-loss strategy, you want to see if low-carb eating beneficially changes your blood sugar profile over the course of the day.
Who should not consider a CGM:
- You are uninterested or unwilling to change your lifestyle.
- You are cost-sensitive and content checking blood sugar once or twice daily.
- You are pregnant, critically ill, or on dialysis. Most company websites state their devices have not been tested and are not appropriate for use with these groups.5
- You have a high likelihood of becoming obsessive about the blood sugar reading and engaging in unhealthy dietary practices to achieve a particular glucose level.
Who should use caution with a CGM?
- You are taking aspirin, acetaminophen, high-dose vitamin C, or a medication called hydroxyurea. Use caution since these medications can make CGM readings inaccurate. The interactions differ for each manufacturer, so make sure to read the warnings for your specific device.
3. How to use a CGM to monitor blood sugar




There are multiple ways to use a CGM if you want to learn more about your metabolic health and your body’s response to lifestyle choices. Here are a few ways to use the device.
1. Make every meal a chance to learn your carb tolerance
You can think of this as your “real world” glucose tolerance test — literally, how does your glucose level respond to the food you eat?6
- First, check your blood sugar before you eat. This is your baseline level.
- Next, eat a regular meal, or you can design specific meals to test.
- Record your blood sugar values at 30, 60, 90, and 120 minutes after eating.
- Ideally, you want your peak post-meal blood sugar to be less than 140 mg/dL (7.8 mmol/L).
- For people seeking further optimization of their metabolic health, there are a few, small studies using CGM in people without diabetes showing they tend to spend the majority of their time below 120 mg/dL (6.7 mmol/L).7
If your blood sugar responds as described, congratulations! You respond well to your chosen meal and can eat it as part of a metabolically healthy diet.
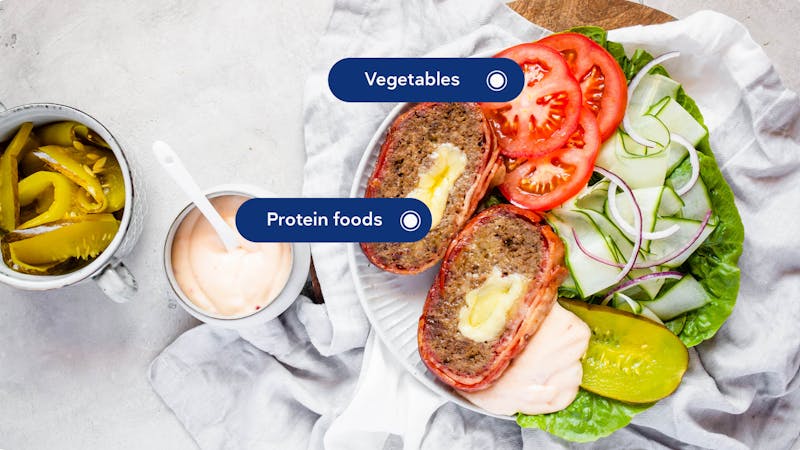
If your blood sugar is higher than desired or consistently takes longer than 2 hours to return to baseline, then try switching up your chosen meal and test again. Consider reducing the number of carbohydrates or add fat and protein to blunt the carbs’ effect.
For example, eating berries alone will likely cause a greater and faster blood sugar rise than eating berries with whipped cream. And eating spaghetti with meatballs will affect your blood sugar more than will zoodles with Bolognese sauce.
2. Make every day a chance to improve your average glucose levels
CGMs calculate your average glucose levels every day, which is more immediate than what a HbA1c test represents (a three month average of blood sugars).
Additionally, interpretation of a HbA1c test result is based on the assumption that red blood cells live 120 days — but this is actually just a rough estimate. Red blood cell lifespan may vary from person to person, which can affect the A1c result. In addition, there are several factors other than blood sugar that can raise or lower the A1c, making CGM a useful complementary tool.8
A “normal” average daily glucose level is less than 114mg/dL (6.3 mmol/L), which correlates with an A1c of 5.6% (37 mmol/mol).9
However, numerous studies show higher HbA1c levels correlate with an increased risk of poor health outcomes. Although it is not well studied, it is possible that it is even better to average below 100 mg/dL (5.6 mol/L), which correlates to an A1c of 5.0% (31 mmol/mol).10
3. Make each day a sleep and stress test
Food isn’t the only variable that affects your blood sugar.
Poor sleep and poorly managed stress can increase blood sugar levels, regardless of how well you eat.11 Exercise and intermittent fasting, on the other hand, can improve your blood sugar levels.12
Kara Collier, RD, co-founder and director of nutrition at Nutrisense.io, says sleep and stress impact blood sugar readings far more than most people think.
In her clinical experience, she sees up to a 25% variation in blood sugar levels depending on variable sleep habits and stress levels. And it isn’t just the amount of sleep that has an impact. Not getting enough REM or deep sleep can also impact blood sugar readings the next day.
Collier’s number one way to tell if chronic stress is negatively impacting someone’s blood sugars is if their weekend levels are much better than their weekday levels, despite no change in diet.
For those individuals, who may experience a stressful workweek, mindfulness practice may have a more significant blood sugar impact than different food choices.
It may be difficult to pinpoint one specific variable since you can’t always control your sleep, your stress, and all your meals. But the more detailed notes you keep, the more information you have to act upon.
Not a fan of taking notes? Don’t get discouraged!
Even without taking notes, you will learn a great deal just by wearing a CGM and paying attention to the trends.
4. Why is a CGM better than other methods of monitoring blood sugar?




A CGM gives you constant accountability. It’s like a diet coach on your upper arm, reminding you to think before you eat.
Many individuals report better dietary compliance simply because they don’t want the negative feedback of a visible glucose rise.13
Behavioral change can be difficult. The added accountability that comes with wearing a CGM may be what you need to succeed long term.
Fasting blood sugar is the most commonly used blood sugar measurement in typical medical practices. Unfortunately, it is likely also the least helpful for early detection of metabolic disease.14
For this reason, tracking blood sugar variations throughout the day with a CGM provides the opportunity to detect problems earlier.15
Studies suggest that glucose variability may be a better predictor of metabolic health than fasting blood sugar.16
Another study using CGMs reported that a low glucose trough three hours after eating correlated with increased hunger and calorie intake at the next meal.17 Although correlation does not prove causation, these findings suggest another way in which CGMs can help inform your food choices.18
The bottom line is that having immediate, real-time feedback provides valuable and actionable information.19
5. Downsides of CGMs
#1: Lag/accuracy
CGMs measure glucose in the tissue fluid just under your skin, called interstitial fluid. Interstitial fluid glucose levels can lag behind blood glucose levels by several minutes. Therefore, during a rapid drop or rise in blood sugar, the reading on your CGM may overestimate or underestimate your true blood sugar level, respectively. This can be dangerous if making an insulin dosing decision based off the CGM reading.
Newer CGM models have better accuracy than previous models but still have around a 10% to 20% error margin depending on which manufacturer’s CGM you use.20
When you start using your CGM, you may still need to do fingerstick glucose checks to understand if your CGM is a little too high, too low, or just right.
Also, studies differ as to the test-to-test accuracy of CGMs. A study by Kevin Hall cast some doubt about the repeatability of the results, whereas another study by Jordi Merino suggested better accuracy.21 As technology continues to progress, we expect the accuracy to improve in step.
#2: Price
CGMs aren’t cheap. Most health insurance policies will only cover them if you are on insulin. Otherwise you will have to pay between $70 and $800 for one month of monitoring.22
For those concerned about cost, you can use a much cheaper blood glucose meter and prick your finger before each meal and two-to-three times after each meal to get similar information at a fraction of the cost.
#3: Obsession
CGMs could trigger an obsessive personality trait in which the user focuses on getting a ”flatline” tracing, meaning no rise in blood sugar.
#4: Missing other factors
CGMs could motivate you to eat in a manner that worsens other health parameters for the sake of your blood sugar. For instance, fat bombs and butter coffee may not affect your blood sugar, but if the extra fat calories add up, they could lead to weight gain and eventual insulin resistance in the future. Keep in mind that blood sugar is one of many health markers to consider.
Healthcare professionals would probably agree that, within a broad, healthy range, lower average blood sugar levels are better than higher ones, and lower variability is a good thing. But there is likely a point of diminishing returns.
For instance, there may not be a meaningful difference between a postprandial glucose level of 105 versus 95. In fact, the difference could simply be due to the standard range of error of the machine.
Maybe your coffee with butter and MCT oil keeps your sugar at 80, but eating an omelet with spinach and cheese increases it to 100.
Are you better off with the nutrient-poor coffee or the higher protein, more nutrient-dense omelet — despite the small increase in blood sugar? It’s important to understand that blood sugar is only one of many considerations for picking the “best” foods for your health.
6. Different CGM options




There are four different options for CGMs currently available, all requiring a prescription in the U.S., although not in Canada and some other areas. Three are sensors you put on yourself, and one requires a doctor to implant it under your skin.
All of the available CGMs are reasonably accurate, but few studies compare the latest devices’ accuracy.23 Currently, some clinicians feel the Dexcom is the most accurate with the Abbott being less accurate, but it isn’t clear that the difference is enough to alter the utility of the devices.24
Cost varies widely among devices with Abbott being the least expensive option.25
- Abbott Freestyle Libre costs around $80 per month with no additional fees. The price makes this a favorite choice among experienced practitioners.
- Dexcom G5 and G6 cost around $350 monthly, with a one time expense of $500.
- Medtronic Guardian costs around $500 monthly, plus a one time expense of $700.
- Senseonics Eversense:26 This particular CGM requires a physician visit for the initial insertion. This sensor can remain in place for 90 days in the US and 180 days in Europe. Cost varies by insurance, but this is likely not a good choice for those paying cash, given the expense of the doctor’s visit.
7. Why is it important to monitor blood sugar?




Checking your blood sugar can keep you on your nutrition plan. Most people don’t want to see a high blood sugar number flashing on their screen, reminding them they ate something that makes their blood glucose go up.
Additionally, the data consistently show that elevated blood sugars are associated with a higher risk of heart disease, heart failure, and other harmful diseases — even without a diagnosis of diabetes.27 But the optimal diet for keeping blood sugar normal may not be the same for everyone.
Studies have shown that seemingly healthy people can have drastically different glucose responses to the same meal. Some may barely see a bump in their blood sugar level, while others may see a significant rise.28 Such variability makes general dietary recommendations less useful for each individual. Instead, a CGM can help you understand what foods help or harm your blood sugar response the most.
Also, CGMs may be the best tools for detecting glucose variability. Higher glucose variability correlates with worse health outcomes and is, therefore, an important measurement to follow.29
8. Next steps: a 4-week plan




First, discuss with your clinician if a CGM is right for you since it requires a prescription, at least in the U.S. If you are looking for a doctor experienced with CGM, consult our find a doctor map.
Week 1: Once you have your CGM, use the first week as a “monitoring” week. Try not to change your lifestyle in any meaningful way. Record and monitor your blood sugar patterns, merely taking notes without reacting to them. If the values are different from what you expected, consider confirming them a few times with a finger stick measurement.
Weeks 2 and 3: During the next two weeks, experiment with different foods to note how they affect your glucose responses. For example, if you notice a peak of 150mg/dL (8.3 mmol/L) after your oatmeal and fruit in the morning, experiment with our scrambled eggs with veggies to see how it compares.30
You can also experiment with combinations of foods. Eating an apple may cause your sugar to increase, but combining it with peanut butter may significantly lower your blood sugar peak.
Once you get a feel for how different foods affect your blood sugar, you can also experiment with exercising before or after eating, going to bed earlier or later, or different lengths of intermittent fasting.
Just remember to change only one thing at a time; otherwise, you will have to guess which action led to the result.
Week 4: During the fourth and final week, implement a new way of eating based on the experiments and compare your results to week one. Hopefully, you have learned which meals you react best to, and you can create a week-long meal plan to try your new way of eating.
Of course, your experiment doesn’t have to end at four weeks. You can choose to continue to wear a CGM long term and continue occasional experiments. But for the sake of simplicity, some prefer to learn as much as possible in four weeks and then start a consistent diet optimized for their glucose response.
9. Summary
A continuous glucose monitor is a more comprehensive blood sugar measuring tool than a traditional glucometer. It provides real-time, actionable feedback that you can use to improve your metabolic health.
The need for a physician’s prescription in the U.S. and some other areas may limit access to CGMs, and cost may be a consideration as most health insurance policies only cover them for people taking insulin.
However, if you want the most detailed analysis of your blood sugar and to learn as much as you can about how different foods impact your metabolic health, a CGM may be the right choice for you.
Do you want to learn more about CGMs? Listen to the Diet Doctor Podcast with Dr. Casey Means, co-founder of Levels Health.
Low-carb video
What is a CGM — and is it right for you? - the evidence
This guide is written by Dr. Bret Scher, MD and was last updated on June 19, 2025. It was medically reviewed by Dr. Michael Tamber, MD on March 12, 2022.
The guide contains scientific references. You can find these in the notes throughout the text, and click the links to read the peer-reviewed scientific papers. When appropriate we include a grading of the strength of the evidence, with a link to our policy on this. Our evidence-based guides are updated at least once per year to reflect and reference the latest science on the topic.
All our evidence-based health guides are written or reviewed by medical doctors who are experts on the topic. To stay unbiased we show no ads, sell no physical products, and take no money from the industry. We're fully funded by the people, via an optional membership. Most information at Diet Doctor is free forever.
Read more about our policies and work with evidence-based guides, nutritional controversies, our editorial team, and our medical review board.
Should you find any inaccuracy in this guide, please email andreas@dietdoctor.com.
JAMA Cardiology 2021: Association of Lipid, Inflammatory, and Metabolic Biomarkers With Age at Onset for Incident Coronary Heart Disease in Women [observational study with HR > 2, weak evidence]
NEJM 2013: Glucose levels and risk of dementia [observational study, weak evidence]
Cancers 2019: Hyperglycemia Associated Metabolic and Molecular Alterations in Cancer Risk, Progression, Treatment, and Mortality [overview article; ungraded]
↩If you are looking for a doctor experienced with CGM, consult our find a doctor map. ↩
Journal of Diabetes Research 2019: Utility of Real-Time and Retrospective Continuous Glucose Monitoring in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Randomized Controlled Trials [ strong evidence] ↩
This is based on the consistent clinical experience of practitioners familiar with low-carb nutrition. [weak evidence] ↩
However, this advice may change as several studies have been done or are in process for validating the use of CGM in these patient populations. ↩
For the following discussion, we are extrapolating data from glucose tolerance tests which traditionally test blood sugar after you ingest 75 to 100 grams of a glucose solution. With “real world” tests on your everyday meals, chances are that you won’t consume 75 to 100 grams of glucose — plus you will be consuming protein and fat along with any carbs — and therefore using GTT cutoffs for meals isn’t precisely valid. Therefore the recommendations in the following section are based on clinical experience, extrapolation, and studies of CGMs in people without diabetes.
The following graphic from the American Diabetes Association summarizes its guideline regarding the interpretation of fasting blood glucose, glucose tolerance tests, and HbA1c levels:
https://www.diabetes.org/a1c/diagnosis
Diabetes Care 2010: Diagnosis and classification of diabetes mellitus [overview article; ungraded]
The following studies reported healthy adults spent less than 1% of their time at levels above 140 mg/dL (7.8 mmol/L)and most of their time below 120 mg/dL (6.7 mmol/L)
.
Journal of DIabetes Science and Technology 2007: Continuous glucose profiles in healthy subjects under everyday life conditions and after different meals [nonrandomized study, weak evidence]Diabetes Care 2010: Variation of interstitial glucose measurements assessed by continuous glucose monitors in healthy, nondiabetic individuals [nonrandomized study, weak evidence] ↩
Biomarker Insights 2016: Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients [overview article; ungraded] ↩
Diabetes Care 2010: Diagnosis and classification of diabetes mellitus [overview article; ungraded] ↩
Many studies suggest that lower is better for reducing the risk of future health conditions, although most do not focus on “optimal” levels and instead focus on levels below diabetes or prediabetes levels.
PLoS One 2015: The impact of diabetes mellitus and corresponding HbA1c levels on the future risks of cardiovascular disease and mortality: a representative cohort study in Taiwan [Observational study with HR > 2, weak evidence]
Journal of the American Heart Association 2013: Hemoglobin a1c is associated with increased risk of incident coronary heart disease among apparently healthy, nondiabetic men and women [Observational study with HR < 2; very weak evidence]
Science Reports 2019: Visit-to-visit HbA1c and glucose variability and the risks of macrovascular and microvascular events in the general population [Observational study with HR > 2, weak evidence]
Diabetes 2010: The association of hemoglobin a1c with incident heart failure among people without diabetes: the atherosclerosis risk in communities study [Observational study with HR < 2; very weak evidence]
↩Sleep:
Sleep Medicine Clinic 2007: Impact of sleep and sleep loss on glucose homeostasis and appetite regulation [overview article; ungraded]Stress:
Annual Review of Public Health 2015: Stress and type 2 diabetes: a review of how stress contributes to the development of type 2 diabetes
[overview article; ungraded] ↩Exercise:
Diabetes, Metabolic Syndrome, and Obesity 2013: The impact of brief high-intensity exercise on blood glucose levels [review of randomized and nonrandomized studies, weak evidence]
Diabetes Care 2016: Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association [overview article; ungraded]
Fasting:
World Journal of Diabetes 2017: Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study [nonrandomized study, weak evidence]
Translational research: Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings [overview article; ungraded]
↩This is based on consistent clinical experience of practitioners who use low-carb diets. [weak evidence] ↩
PLoS One 2020: Diagnostic accuracy of tests for type 2 diabetes and prediabetes: A systematic review and meta-analysis [Meta-analysis of nonrandomized studies, weak evidence]
Diabetes and Metabolic Research Reviews 2013: Use of high-normal levels of haemoglobin A(1C) and fasting plasma glucose for diabetes screening and for prediction: a meta-analysis [Meta-analysis of observational studies, weak evidence]
However, as we detail in our guide about the dawn effect, slightly elevated fasting blood sugar readings can also be misleading, especially for people following a low-carb diet or engaged in intermittent fasting.
This is based on consistent clinical experience of practitioners familiar with low-carb nutrition. [weak evidence] ↩
This study shows “mean amplitude of glucose excursion,” also known as glucose variability, was associated with cardiovascular events — even in patients without diabetes.
Journal of the American Heart Association 2017: Effects of the Mean Amplitude of Glycemic Excursions and Vascular Endothelial Dysfunction on Cardiovascular Events in Nondiabetic Patients With Coronary Artery Disease [nonrandomized study, weak evidence]
The following study and review report postprandial glucose readings (your blood glucose after a meal) significantly improve prediction of cardiovascular risk.
Diabetes Care 2009: Postprandial glucose improves the risk prediction of cardiovascular death beyond the metabolic syndrome in the nondiabetic population [nonrandomized study, weak evidence]
Obesity Reviews 2012: Impact of postprandial glycaemia on health and prevention of disease [overview article; ungraded]
↩Nature Metabolism 2021: Postprandial glycaemic dips predict appetite and energy intake in healthy individuals[randomized trial; moderate evidence] ↩
Choosing foods that do not result in “glucose dips” several hours after eating might be associated with less hunger. ↩
This is based on consistent clinical experience of practitioners who use low-carb diets. [weak evidence] ↩
This review paper discusses the error margins.
Sensors 2016: Continuous Glucose Monitoring Sensors: Past, Present and Future Algorithmic Challenges [overview article; ungraded] ↩
American Journal of Clinical Nutrition 2020: Imprecision nutrition? Different simultaneous continuous glucose monitors provide discordant meal rankings for incremental postprandial glucose in subjects without diabetes[non-controlled study; weak evidence]
American Journal of Clinical Nutrition 2022: Validity of continuous glucose monitoring for categorizing glycemic responses to diet: implications for use in personalized nutrition[non-controlled study; weak evidence] ↩
Pharmacy and Therapeutics 2019: Continuous Glucose Monitoring: A Review of Available Systems [overview article; ungraded] ↩
As mentioned in the previous section, one study found significant variability between brands, while another found the variability was present, but less pronounced:
American Journal of Clinical Nutrition 2020: Imprecision nutrition? Different simultaneous continuous glucose monitors provide discordant meal rankings for incremental postprandial glucose in subjects without diabetes[non-controlled study; weak evidence]
American Journal of Clinical Nutrition 2022: Validity of continuous glucose monitoring for categorizing glycemic responses to diet: implications for use in personalized nutrition[non-controlled study; weak evidence]
Studies of older versions of the devices showed mild variability among devices.
Diabetes Tecnology and Therapeutics 2013: Accuracy and reliability of continuous glucose monitoring systems: a head-to-head comparison [randomized trial; moderate evidence] ↩
Pharmacy and Therapeutics 2019: Continuous Glucose Monitoring: A Review of Available Systems [overview article; ungraded] ↩
Diabetes Technology and Threapeutics 2019: Clinical Practice Recommendations on the Routine Use of Eversense, the First Long-Term Implantable Continuous Glucose Monitoring System [overview article; ungraded] ↩
For example, this study reports an increased risk of heart attacks and death with increasing A1c
PLoS One 2015: The impact of diabetes mellitus and corresponding HbA1c levels on the future risks of cardiovascular disease and mortality: a representative cohort study in Taiwan [Observational study with HR > 2, weak evidence]The same applies even to those without a diagnosis of diabetes.
Journal of the American Heart Association 2013: Hemoglobin a1c is associated with increased risk of incident coronary heart disease among apparently healthy, nondiabetic men and women [Observational study with HR < 2; very weak evidence]
Science Reports 2019: Visit-to-visit HbA1c and glucose variability and the risks of macrovascular and microvascular events in the general population [Observational study with HR > 2, weak evidence]
Diabetes 2010: The association of hemoglobin a1c with incident heart failure among people without diabetes: the atherosclerosis risk in communities study [Observational study with HR < 2; very weak evidence] ↩
Cell 2015:
Personalized Nutrition by Prediction of Glycemic Responses [randomized trial; moderate evidence]PLoS Biology 2018: Glucotypes reveal new patterns of glucose dysregulation [nonrandomized study, weak evidence] ↩
Journal of the American Heart Association 2017: Effects of the Mean Amplitude of Glycemic Excursions and Vascular Endothelial Dysfunction on Cardiovascular Events in Nondiabetic Patients With Coronary Artery Disease [nonrandomized study, weak evidence]
Diabetes and Metabolism Journal 2015: Glycemic Variability: How Do We Measure It and Why Is It Important? [overview article; ungraded] ↩
A pilot study demonstrated the safety and efficacy of using a CGM as part of a low-carb eating plan for those with prediabetes.
JMIR Diabetes 2020: Continuous Glucose Monitoring With Low-Carbohydrate Diet Coaching in Adults With Prediabetes: Mixed Methods Pilot Study [nonrandomized study, weak evidence] ↩