Heavy hips and legs – could you have lipedema?
Do you have big legs, thighs, hips, upper arms, or saddlebags? Do they seem out of proportion to the rest of your body? Are they painful, or do they bruise easily?
If you answered “yes” to any of these questions, you may have lipedema (spelled lipoedema in the UK and Europe.) Lipedema is the disproportionate accumulation of fat in the lower body that primarily affects women. Often that fat is painful.
Your upper body may respond to diet and exercise or be quite normal in size, but from the waist down, you may have lumpy legs with excess fat that is frustratingly impossible to lose.
You’re hoping to find answers for how to lose weight with lipedema or to stop the growing accumulation of painful fat on your hips and legs.
Don’t worry. You’ve come to the right place. This guide will help you better understand what is known about lipedema, a complex and often misdiagnosed female condition.1 In addition, our companion feature article explores women’s inspiring anecdotal experiences with the ketogenic diet for lipedema.

1. What is lipedema?
Lipedema is a chronic, progressive condition (meaning it worsens over time) of disordered fat metabolism.When it was first described in 1940 it was defined as the disproportionate and symmetrical accumulation of adipose [fat] tissue on the lower half of the body combined with fluid retention.2
While the name combines the medical words “lip” (fat) and “edema” (swelling caused by excess fluid), the role of fluid retention from the lymphatic system in the early stages of lipedema has recently become controversial. Some have even argued the name should be changed to lipalgia, for painful fat.3




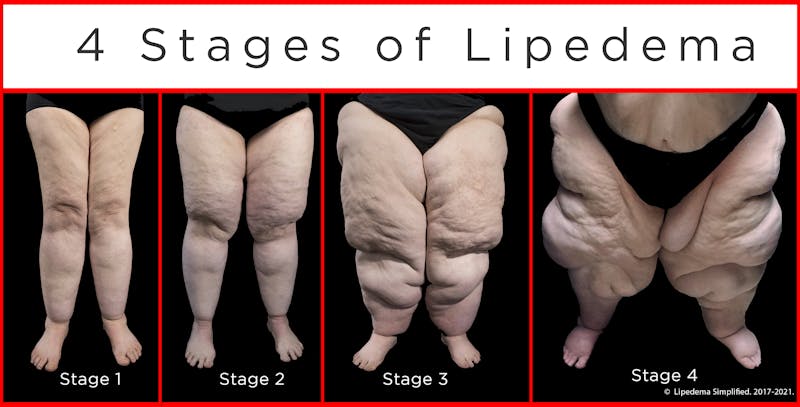
Image ©2017-2021.Lipedema Simplified, LLC. All rights reserved. Used with permission.
What is not controversial, however, is that if the disease progresses to later stages, with increasing obesity, blocked flow of lymph fluid can cause the legs to swell. That’s called secondary lymphedema.4
2. Is lipedema just obesity?
No. Obesity and lipedema are seen as two separate conditions that often occur together (comorbidities), with an estimated 80% of women with lipedema also being overweight or obese.5If you are obese, your lipedema symptoms may be more pronounced. Likewise, if you have the inherited tendency to develop lipedema, you may gain weight and accumulate fat tissue more easily than others. The current view is that it is a vicious cycle between the two conditions.6
How many women have lipedema? The evidence is conflicting, with recent estimates ranging from less than 5% to up to 18%. Some researchers say the average is likely about 10% of all women.7
Yet, many in the medical profession still don’t recognize the condition. That means women with lipedema may take more than 20 years to get a proper diagnosis. Many are told that they simply have a female, pear-shaped form of obesity.
Have you had your concerns about your heavy legs and your symptoms dismissed and been told to restrict calories and exercise more? You are not alone.
Many women with lipedema have been made to feel guilty and ashamed that they have caused their condition by overeating and being lazy. They are often told they need to try even harder to diet and exercise to lose weight.8
Some women do just that: exercise and diet constantly, only to have their painful legs continue to grow in size and heaviness. As a result, women with lipedema experience higher than average rates of eating disorders, anxiety, depression, low self-esteem, and appearance-related distress.9
Up until recently, lipedema has been largely ignored by scientific research and clinical trials, despite its toll on the physical and emotional health of the women it impacts.
Fortunately, lipedema was finally given a classification and an international disease code when it was added to the World Health Organization’s International Classification of Diseases (ICD-11) in September 2020. It is hoped that this will lead to more women getting an accurate and timely diagnosis.
Summary
Lipedema is a complex female disorder of painful fat accumulation on the lower body. The condition is often misdiagnosed as simply a female form of obesity, which contributes to the high rates of eating disorders, self-blame, anxiety, depression, and appearance-related distress among women with the condition.3. Main symptoms
All women with lipedema have disproportionate fat accumulation in their lower bodies. Other symptoms are common, but not every woman has them. Other symptoms may include:10- Painful fat: The fat on the legs and hips may ache and be sensitive or painful to the touch or to any pressure. In the past, sometimes the condition was called adiposis dolorosa, meaning “painful fat.”
- Easy bruising: The legs and hips may be easily bruised, even with the slightest bump. Tiny spider veins (telangiectasia) may be close to the surface, contributing to bruising.
- Upper arm fat: About 30% of women with lipedema also have excess fat collecting in their upper arms.
- Hard nodules: If the fat is massaged, pea-sized hard lumps can often be felt under the skin.
- Cuffing at the ankle or wrist: Since the feet and hands are unaffected, the swollen legs can get a cuff-like appearance, especially in later stages of the condition.
- Edema: While the role of edema is controversial, in the early stages of lipedema, women can experience swelling of their legs as the day goes on, particularly if on their feet all day (orthostatic edema).
- Cold skin: Sometimes, the skin of the legs and hips are cooler to the touch than other parts of the body or in comparison to women without the condition.
- Hypermobile joints: Joints may have a greater range of motion than average, which can contribute to joint damage, pain, and walking issues.
Later stage symptoms
- Lymphedema: As the condition progresses, obesity-related lymphedema can occur, in which the flow of lymph fluid is obstructed, causing the limbs to swell with fluid.11
- Difficulty walking: Over time, leg size, pain, and heaviness can cause joint damage and gait changes, interfering with walking and leading to immobility.
- Fibrosis: Over time, likely due to chronic inflammation, ropy scar tissue can form among the leg fat. Called fibrosis, this scarring likely contributes to further hampering of lymph circulation.
Miscellaneous related symptoms
Recent studies have found that compared to other women, women with lipedema tend to have higher rates of hypothyroidism, migraines, and depression.12
Despite having body mass indexes (BMI) that are often in the obese range, women with lipedema have lower rates of type 2 diabetes, high blood pressure, and metabolic syndrome — likely because the fat is primarily located on their hips and legs and not around their waist and visceral organs.13
Summary
The main symptom of lipedema is disproportionate fat on the hips and legs. Other common symptoms include pain, easy bruising, cuffing of the legs or arms, hard nodules that can be felt under the skin, upper arm fat, and leg swelling.4. What causes lipedema?
The cause of lipedema is unknown. It is believed to have a strong inherited component since at least 60% of women with lipedema have a female relative, such as a mother, sister, or grandmother, with large, painful hips and legs.14Lipedema arises at times of hormonal change, particularly puberty, pregnancy, and menopause, and is thought to be related to changes in estrogen levels and perhaps to periods of life that are marked by higher circulating insulin (hyperinsulinemia.)15
A number of genes may be involved, likely having to do with adipose (fat) tissue storage, the lymphatic system, and sex hormone metabolism. The first potential gene linked to lipedema was discovered in 2020, involved with the metabolism of the sex hormone progesterone.16
What goes wrong in lipedema? For an unknown reason, dysfunctional fat cells accumulate disproportionately on the woman’s hips, legs, and sometimes on their upper arms. The waist, torso, face, neck, hands, and feet are largely unaffected.17
As noted, while the role of the lymphatic system in the disorder is controversial, there is some evidence that as the fat accumulates, lymph vessels among the fat tissue leak fluid, which then attracts the creation of more fat cells around the stagnant lymph, and then more lymph leakage and swelling, creating a vicious cycle.18
In recent years, a number of other cellular differences have been found between women who have lipedema and healthy women who don’t. These include the size of fat cells, and the salt content, oxygenation, and inflammatory markers inside the fat cells.
The full picture of how these cellular differences contribute to lipedema’s cause and symptoms is still to be determined.
Summary
The cause of lipedema is unknown, but the condition has a strong genetic component and a relationship to changes in sex hormone levels. Recent research is showing a number of microvascular and cellular differences are likely part of the lipedema picture.5. Diagnosis, type, and staging of lipedema
No laboratory tests or diagnostic imaging exams currently exist to confirm lipedema.Instead, the diagnosis of lipedema is made from the woman’s medical and family history, as well as a physical examination to see how many of the common symptoms she may have.
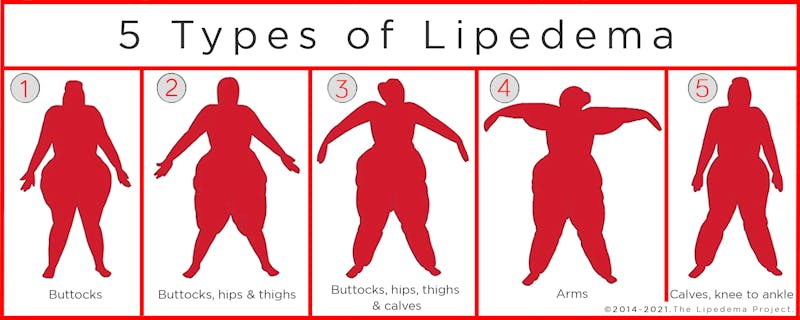
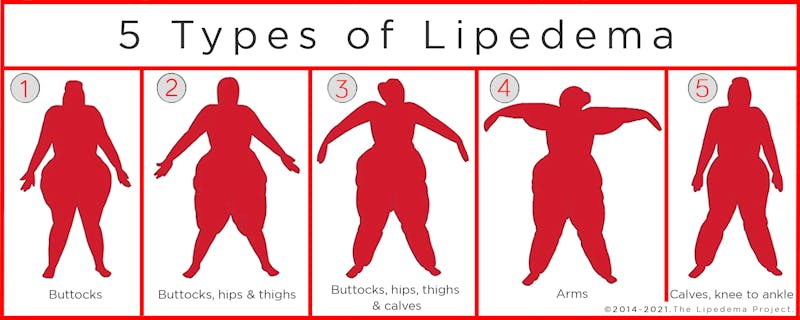
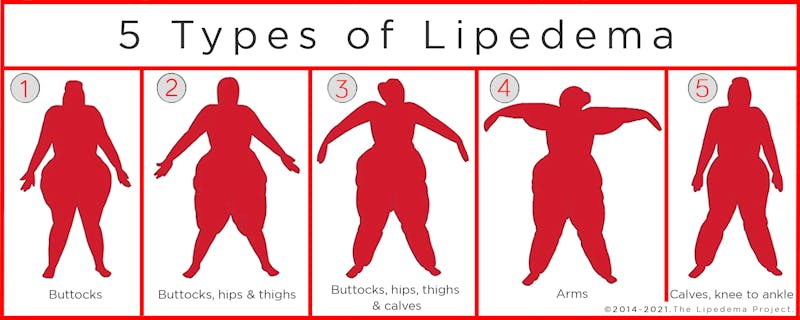
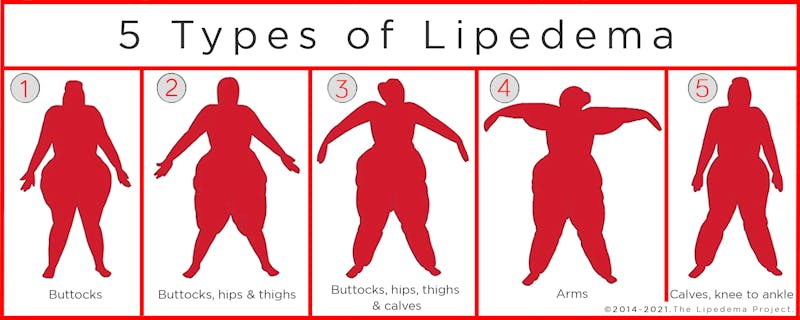
The diagnosis of lipedema is usually described as one of five types, depending on where the excess fat accumulates. Type 1 is the buttocks, hips, and pelvis. Type 2 is from the buttock to the knees. Type 3 is buttocks to the ankles. Type 4 includes the addition of the upper arms. Type 5 is only the lower legs.
The diagnosis also includes one of four stages of progression, depending on how advanced the condition is and the amount of fat accumulation, pain, and lymph involvement
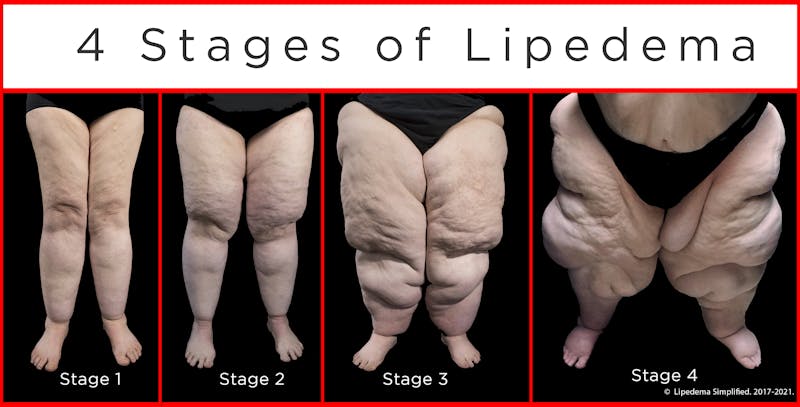
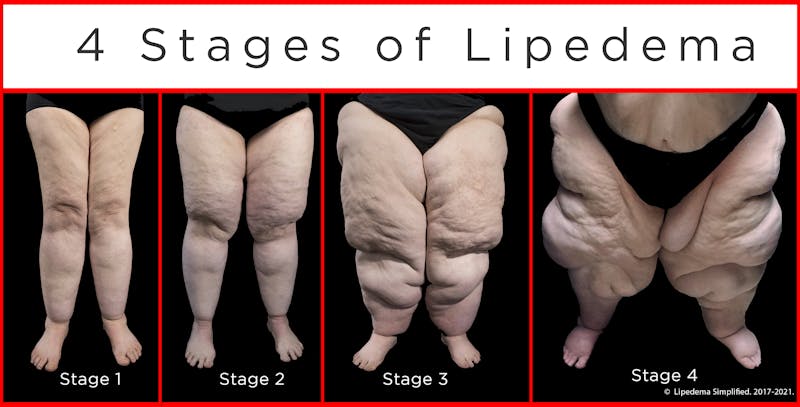
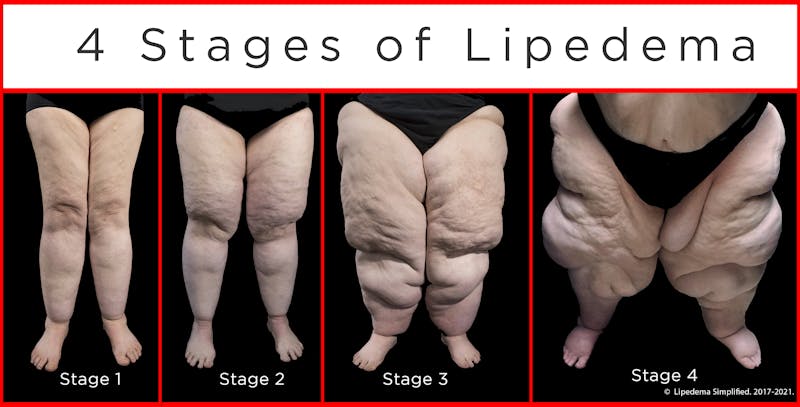
Summary
The diagnosis of lipedema is based on the woman’s medical history and a clinical examination. The condition is classified into one of five types, depending on where the fat is located. The stage of lipedema is noted from 1 to 4, based on the progression of fat accumulation and fluid retention.6. How to lose weight with lipedema
Until recently, lipedema has been seen as almost completely resistant to weight loss through traditional forms of diet and exercise.One of the diagnostic criteria in a woman’s medical history is that she has been unable to lose fat from her hips and legs, while being able to trim down the upper half of her body.
Even bariatric surgery, in which the size of the stomach is reduced, may not be fully effective. Women may lose significant amounts of weight but still have excessive, painful fat in their legs and hips.24
One reason women with lipedema often struggle to lose weight could be that many spend years yo-yo dieting and reducing calories in an attempt to reduce their lower-body fat.25
What might help women to lose lipedema fat, reduce pain, and reduce fluid retention without lowering metabolism? Perhaps the ketogenic diet.26
7. Ketogenic diet




Can the ketogenic diet help with lipedema’s stubborn fat and symptoms, such as pain and fluid retention?
Evidence to date is scant and preliminary. However, a few small studies, as well as a growing body of anecdotal evidence and clinical experience, suggest that it might help.
Read our companion feature article on the growing number of women with lipedema who are doing the ketogenic diet and experiencing weight loss and a reduction in their symptoms.
A small study in California looked at the effectiveness of a ketogenic diet among 12 obese individuals (11 women and one man) who had secondary lymphedema. The study found that restricting carbohydrates and being in ketosis led not only to weight loss but to reduced lymph fluid retention, a significant reduction in the size of the swollen limbs, and improved quality of life for the participants.27
Norwegian researchers have now registered a randomized control trial of a ketogenic diet for lipedema at clinicaltrials.gov. The study title is Effect of Ketosis on Pain and Quality of Life in Patients With Lipedema (Lipodiet).
The study aims to recruit 80 Norwegian women with lipedema by 2023 and randomly assign them for 10 weeks to one of three diets, two of which are ketogenic, and a third, not ketogenic.
Pain and quality of life will be measured at the start and immediately after the intervention. The hypothesis is that a ketogenic diet may be an effective treatment to reduce pain and improve the quality of life for women with lipedema.
Why ketosis may help lipedema
A number of theoretical, physiologic reasons suggest why a ketogenic diet may help with the fat accumulation, pain, and swelling of lipedema.
A 2021 paper by lipedema experts in the journal Medical Hypotheses reviewed the research evidence about lipedema and summarized why a ketogenic diet may help with weight loss, pain, mood, inflammation, preventing progression, and more.28
Some of the research evidence why a ketogenic diet may help includes:
- Effective weight loss: Many studies confirm that in general populations when people dramatically cut back on carbs but are allowed as much protein and fat as they need to feel full, they eat less and lose weight.29 For women with lipedema, the metabolic shifts that occur from burning glucose to burning fat on a ketogenic diet may allow their body to finally access and use their stored lower body fat.
- Reducing insulin: Studies show that women with lipedema have lower rates of type 2 diabetes despite obesity with a high body mass index, which is presumed to mean they are still insulin sensitive.30 However, at a cellular level, the fat that is stored on their hips and legs seems to be more resistant to insulin’s action.31 Additionally, the condition arises at times when women are physiologically more insulin resistant (during puberty, pregnancy, and menopause). Insulin is like a key in a lock that opens fat stores to be accessed for fuel. Insulin resistance prevents that key from working. A ketogenic diet reduces insulin levels, which allows the fat stores on the limbs to be opened and fat to be accessed for fuel (called lipolysis).32
- Pain reduction: A number of studies have shown that a ketogenic diet reduces joint pain and chronic pain in people with obesity, and other pain conditions, that are unrelated to weight loss alone.33 The pain of lipedema fat could be reduced by a number of mechanisms, one of which is reducing inflammation. Growing anecdotal and clinical evidence is showing this pain reduction can be profound and may occur within a couple of days of starting the diet, long before any weight loss has occurred.
- Removal of excess fluid: In the first few days of a ketogenic diet, people lose water weight. This is because glucose stored in muscles (called glycogen) holds onto water and when that is depleted water is lost.34 This is called the diuretic effect of eating a low-carbohydrate diet. The water loss from tissues could help women with lipedema reduce their water retention. As noted above, a small study found that for people with obesity and lymphedema, a ketogenic diet was effective at reducing weight, and the size and amount of retained lymph fluid in their affected limbs.35
- Removal of excess salt: A ketogenic diet, by lowering insulin and releasing water weight, also shifts salt out of the body.36 This may be beneficial for women with lipedema who have been shown to have higher sodium concentrations in the fat tissue of their hips and legs.37
- Decreasing inflammation: Studies have shown that ketogenic diets reduce a number of inflammatory markers.38 Ketosis may help reduce the markers of inflammation that have been found in the fat tissue of women with lipedema.
- Improving mental well-being: A ketogenic diet has been found in a few studies to improve mental clarity and decrease anxiety and depression.39 This impact could help improve the quality of life of women with lipedema.
Clinical experience
To date, clinical experience with the ketogenic diet and lipedema is extremely limited. However, many lipedema experts recommend that women with lipedema avoid eating any added sugar, high glycemic foods, and processed foods. This means most lipedema experts are already supporting a lower-carbohydrate diet in principle.40
One lipedema clinic in Germany has been using a protein-optimized ketogenic diet as therapy for women with lipedema for more than 10 years.41
Dr. Gabriele Faerber, of the Center for Vascular Medicine in Hamburg, Germany, presented her clinical findings to a virtual symposium on ketogenic diets for lymphatic/fat disorders in November 2020. While her results are not yet published in a journal, Dr. Faerber conducted a follow-up study of 100 lipedema patients who used the ketogenic diet for an average of three years. The majority of women who maintained a keto diet experienced weight loss, pain reduction, decreased leg circumference, and improved quality of life.
Dr. Faerber noted lipedema patients need to treat the ketogenic diet and carbohydrate restriction as a life-long behavior change to prevent a relapse of symptoms or progression of lipedema.
Also, at the November 2020 symposium on the ketogenic diet for lymphatic/fat disorders, a number of women with lipedema presented their positive experiences with keto eating. Some shared weight loss of more than 100 pounds (45 kilos) and complete resolution of their pain within a few days of starting ketogenic eating, often long before they lost any weight.
The organization Lipidema Simplified offers a membership group (Lipedema TRIBE Community), educational workshops, webinars, and online support groups — and has served over 50,000 women with lipedema since 2012.
An associated private Facebook group, Keto WOE [Way of eating] for Lipedema, has more than 11,000 members with many reporting significant weight loss and improvement in symptoms.
More high-quality studies, such as randomized controlled trials, are needed.
Read more about women’s anecdotal experiences with the ketogenic diet for lipedema in our companion article.
Summary
A few small studies about the ketogenic diet for lipedema have been promising, a randomized clinical trial is underway, and a theoretical grounding exists for the diet’s possible effectiveness. Emerging clinical experience, as well as women’s stories, are encouraging.8. Other treatments
Women with lipedema may have some of their symptoms improve by a few other evidence-based treatments:- Exercise : Keeping active and doing even gentle movement can help with the flow of lymph fluid, limb size, improve mental health, and potentially assist weight maintenance.43 Aquatic exercise, such as walking or moving in water, is particularly beneficial as it protects the joints and adds additional support for the body. The force of the water also applies light compression to the legs, which helps lymph movement. Women with lipedema also use rebounders (small trampolines) or exercise on vibration plates.44
- Compression: Wrapping legs with compression bandages or special compression velcro wraps, or wearing flat-knit compression hose, can help improve the pain, mobility, and lymph flow in the limbs.45 As well, some women find symptom improvement and decreased leg swelling from the use of intermittent pneumatic compression, a device with a leg cuff that rhythmically massages the legs.46
- Manual lymph drainage: Used most often for people who develop lymphedema following cancer treatments, manual lymph drainage (MLD) is a form of gentle, rhythmic massage in the direction of lymph flow. It is usually conducted by trained therapists, but you can be taught to do it yourself on your own limbs. In use for lymphedema since the 1930s, MLD as a treatment for lipedema has recently been called into question by some.
However, past studies have found it decreases pain and depression, helps with swelling, and improves quality of life in women with lipedema.47 Recently, adding a vibration plate (which shakes the leg tissue) with MLD has shown additional benefits in improved symptoms and quality of life.48
- Liposuction: Physically removing the lipedema fat from the legs and hips with liposuction is controversial, with some experts saying it is not helpful, has a poor research evidence base, and may be harmful.49 However, other experts counter that liposuction, conducted by clinics specializing in lipedema, has an acceptable research history and has been shown to reduce the leg size and pain of lipedema.50
Summary
Women with lipedema may be helped by other evidence-based therapies including exercise, compression, manual lymph drainage, and potentially liposuction from specialized lipedema clinics.Conclusion
Lipedema is a complex, misunderstood condition of disproportionate storage of often painful fat on the hips and legs of genetically susceptible women.Obesity is a common aggravating factor in lipedema’s symptoms, but the two conditions, obesity and lipedema, are considered to be separate but related in what may be a vicious cycle.
So if you have lipedema you may have been misdiagnosed as just having a female form of obesity and made to feel responsible for eating too much and exercising too little. Traditionally, however, the condition has been deemed resistant to most diets and exercise.
The chronic progressive nature of the condition, which can lead in later stages to immobility and limb swelling from a dysfunctional lymphatic system, contributes to women’s eating disorders, anxiety, depression, and appearance-related distress.
Recently, a ketogenic diet has been proposed as a treatment for lipedema, with a few small promising studies and a strong theoretical basis. Emerging clinical evidence, and anecdotal evidence from increasing numbers of women with lipedema doing the keto diet, is encouraging but more studies are needed.
Other treatments to help improve the symptoms of lipedema include aquatic exercise, compression (with or without the addition of vibration therapy), manual lymph drainage, and liposuction.
Read our companion news features about the growing numbers of women with lipedema who are trying the ketogenic diet. Their impressive results and support are encouraging other women with the condition to try it to lose weight and reduce symptoms, especially pain.
Health
Heavy hips and legs – could you have lipedema? - the evidence
This guide is written by Anne Mullens, Dr. Bret Scher, MD and was last updated on June 19, 2025. It was medically reviewed by Dr. Bret Scher, MD on April 6, 2021.
The guide contains scientific references. You can find these in the notes throughout the text, and click the links to read the peer-reviewed scientific papers. When appropriate we include a grading of the strength of the evidence, with a link to our policy on this. Our evidence-based guides are updated at least once per year to reflect and reference the latest science on the topic.
All our evidence-based health guides are written or reviewed by medical doctors who are experts on the topic. To stay unbiased we show no ads, sell no physical products, and take no money from the industry. We're fully funded by the people, via an optional membership. Most information at Diet Doctor is free forever.
Read more about our policies and work with evidence-based guides, nutritional controversies, our editorial team, and our medical review board.
Should you find any inaccuracy in this guide, please email andreas@dietdoctor.com.
In men, it only occurs in rare conditions where they have high estrogen and low testosterone levels. American Journal of Medical Genetics 2010: Lipedema: An inherited condition [review article; ungraded] ↩
Annals of Internal Medicine 1951: Lipedema of the legs; a syndrome characterized by fat legs and edema [review article; ungraded] ↩
Journal of Wound Care 2020: Lipoedema: a paradigm shift and consensus [expert review; ungraded]
Obesity 2019: Dilated blood and lymphatic microvessels, angiogenesis, increased macrophages and adipocyte hypertrophy in lipedema thigh skin and fat tissue [case-control study; weak evidence] ↩
Secondary lymphedema in lipedema is also now being called advanced stage lipolymphedema.
Cureus 2020: Lipedema and the evolution to lymphedema with the progression of obesity [case series; weak evidence] ↩
Journal of Wound Care 2020:Lipoedema: a paradigm shift and consensus [expert review; ungraded] ↩
American Journal of Medical Genetics 2010: Lipedema: An inherited condition[review article; ungraded]
Obesity (Silver Spring)2019: Lipedema: A call to action[expert review; ungraded] ↩
Plastic and Reconstructive Surgery Global Open 2016: Lipedema: A relatively common disease with extremely common misconceptions[expert review; ungraded] ↩
Obesity (Silver Spring)2019: Lipedema: A call to action[expert review; ungraded] ↩
Psychological Health Medicine 2018: Depression and appearance-related distress in functioning with lipedema [online survey; very weak evidence]
Eating and Weight Disorders 2020: The effect of lipedema on health-related quality of life and psychological status: a narrative review of the literature [review article; ungraded]
BMC Women’s Health 2021: Quality of life, its factors, and sociodemographic characteristics of Polish women with lipedema [online survey; very weak evidence] ↩
Plastic and Reconstructive Surgery Global Open 2016: Lipedema: A relatively common disease with extremely common misconceptions [expert review; ungraded]
Deutsches Arzteblatt International 2020: Lipedema-pathogenesis, diagnosis, and treatment options [expert review; ungraded] ↩
Cureus 2020: Lipedema and the evolution to lymphedema with the progression of obesity;[case series; weak evidence] ↩
Plastic and Reconstructive Surgery 2019: New insights on lipedema: the enigmatic disease of the peripheral fat [expert review; ungraded] ↩
Hormonal, Molecular and Biological Clinical Investigations 2019: Lipedema: friend and foe [overview article; ungraded]
Plastic and Reconstructive Surgery 2019: New insights on lipedema: the enigmatic disease of the peripheral fat [expert review; ungraded] ↩
European Review of Medical and Pharmacologic Science 2019: Genetics of lipedema: new perspectives on genetic research and molecular diagnoses [overview article; ungraded] ↩
Deutsches Arzteblatt International 2020: Lipedema-pathogenesis, diagnosis, and treatment options [expert review; ungraded] ↩
International Journal of Molecular Science 2020: Aldo-keto reductase 1C1 (AKR1C1) as the first mutated gene in a family with nonsyndromic primary lipedema [genetic study;ungraded] ↩
Obesity (Silver Spring)2019: Lipedema: A call to action [expert review; ungraded] ↩
The lymphatic system is a network of tissues, vessels, and organs that work together to move a colorless, watery fluid called lymph around your body into your bloodstream. The lymphatic system has many functions, including protecting your body from infection, maintaining body fluid levels and blood pressure, absorbing digestive tract fats, and removing cellular waste.
Obesity Review 2017: A vicious cycle in chronic lymphoedema pathophysiology? An adipocentric view [overview article; ungraded]
Lymphology 2001: Microlymphatic aneurysms in patients with lipedema [non-controlled study; weak evidence]
Nature Genetics 2005: Lymph makes you fat [expert review article; ungraded]
Cureus 2020: Lipedema and the evolution to lymphedema with the progression of obesity;[case series; weak evidence] ↩
Journal of Surgical Research 2020: Adipose tissue hypertrophy, an aberrant biochemical profile and distinct gene expression in lipedema [non-controlled study; weak evidence]
Obesity 2019: Dilated blood and lymphatic microvessels, angiogenesis, increased macrophages and adipocyte hypertrophy in lipedema thigh skin and fat tissue [case-control study; weak evidence] ↩
Obesity (Silver Spring) 2018: Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema [case-control study, weak evidence]
Obesity (Silver Spring) 2020: Upper and lower extremity measurement of tissue sodium and fat content in patients with lipedema [case-control study, weak evidence] ↩
Obesity 2019: Dilated blood and lymphatic microvessels, angiogenesis, increased macrophages and adipocyte hypertrophy in lipedema thigh skin and fat tissue [case-control study; weak evidence] ↩
Physiology Reviews 2013: Hypoxia and adipose tissue function and dysfunction in obesity [overview article; ungraded]
Journal of Clinical Endocrinology and Metabolism 2016: Adipose tissue hypoxia, inflammation, and fibrosis in obese insulin-sensitive and obese insulin-resistant subjects [non-controlled study; weak evidence] ↩
In the future, a blood test that looks for this protein could potentially be a way of diagnosing lipedema.
Journal of Clinical Insight 2020: Platelet factor 4 is a biomarker for lymphatic promoted disorders [non-controlled study; weak evidence] ↩
Clinical Obesity 2018: Lipoedema in patients after bariatric surgery: report of two cases and review of the literature [very weak evidence] ↩
This could result in the slowing of their metabolism and the reduction of their thyroid function, called famine response hypothyroidism.
Bulletin of the New York Academy of Medicine 1973: Semistarvation: an overview of an old problem [overview article; ungraded]
Physiology and Behavior 2013: Biological mechanisms that promote weight regain following weight loss in obese humans [overview article; ungraded] ↩
Medical Hypotheses 2021: Ketogenic diet as a potential intervention for lipedema [overview article; ungraded] ↩
American Journal of Lifestyle Medicine 2017: Lifestyle modification group for lymphedema and obesity results in significant health outcomes [case series;very weak evidence] ↩
Medical Hypotheses 2021: Ketogenic diet as a potential intervention for lipedema [overview article; ungraded] ↩
Annals of Internal Medicine 2005: Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes [non-randomized trial; weak evidence]
Annals of Internal Medicine 2014: Effects of low-carbohydrate and low-fat diets; a randomized trial [moderate evidence]
The Journal of Clinical Endocrinology and Metabolism 2005: The role of energy expenditure in the differential weight loss in obese women on low-fat and low-carbohydrate diets [randomized trial; moderate evidence] ↩
Hormonal, Molecular and Biological Clinical Investigations 2019: Lipedema: friend and foe [overview article; ungraded] ↩
Trends in Endocrinology and Metabolism 2015: Insulin resistance and impaired adipogenesis[overview article; ungraded] ↩
Current Nutrition Reports 2018: Nutritional ketosis for weight management and reversal of metabolic syndrome [expert review article; ungraded] ↩
Journal of Child Neurology 2013: Ketogenic diets and pain .[expert review article; ungraded]
Frontiers of Neurology 2020: Impact of a ketogenic diet on sporadic inclusion body myositis: A case study[case report; very weak evidence] ↩
The American Journal of Clinical Nutrition 1992:Glycogen storage: illusions of easy weight loss, excessive weight regain, and distortions in estimates of body composition [non-controlled study; weak evidence] ↩
American Journal of Lifestyle Medicine 2017: Lifestyle modification group for lymphedema and obesity results in significant health outcomes [case series;very weak evidence] ↩
Diabetologia 1981: The effect of insulin on renal sodium metabolism. A review with clinical implications[expert review article; ungraded] ↩
Obesity (Silver Spring) 2018: Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema [case-control study, weak evidence]
Obesity (Silver Spring) 2020: Upper and lower extremity measurement of tissue sodium and fat content in patients with lipedema[case-control study, weak evidence] ↩
Frontiers of Endocrinology 2019: Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: A 2-Year Non-randomized Clinical Trial [case report; very weak evidence] ↩
Reviews in the Neurosciences 2020: Exploring the mechanisms of action of the antidepressant effect of the ketogenic diet. [expert review article; ungraded] ↩
British Journal of Community Nursing 2017: Best practice guidelines for the management of lipoedema [expert review article; ungraded]
Deutsches Arzteblatt International 2020: Lipedema-pathogenesis, diagnosis, and treatment options [expert review; ungraded]
Nutrients 2021: Potential effects of a modified Mediterranean diet on body composition in lipoedema [case control study;weak evidence] ↩
The clinic’s protein-optimized ketogenic diet consisted of 1.2 to 1.5 grams of protein daily for every kilogram of ideal body weight, less than 50 grams of total carbs a day, and four handfuls of above-ground vegetables daily. ↩
Single-practitioner experience, very weak evidence. ↩
Lymphatic Research and Biology 2020: The effects of complete decongestive therapy or intermittent pneumatic compression therapy or exercise only in the treatment of severe lipedema: a randomized controlled trial [moderate evidence] ↩
Lymphology 2020: Physiotherapy and rehabilitation applications in lipedema management: A literature review [expert review; ungraded] ↩
British Journal of Community Nursing 2020: Survey of lipoedema symptoms and experience with compression garments [case-control study; weak evidence]
Journal of Wound Care 2020: Lipoedema: a paradigm shift and consensus [expert review; ungraded]
British Journal of Community Nursing 2017:Haddenham easywrap as part of self-management in lymphoedema and lipoedema: The patient perspective [case-series; weak evidence] ↩
Lymphatic Research and Biology 2020: The effects of complete decongestive therapy or intermittent pneumatic compression therapy or exercise only in the treatment of severe lipedema: a randomized controlled trial [moderate evidence]
Lymphology 2012: Intermittent pneumatic compression therapy: a systematic review [moderate evidence] ↩
Journal of Wound Care 2020: Lipoedema: a paradigm shift and consensus [expert review; ungraded] ↩
Physiotherapy Theory and Practice 2020: Low-frequency vibrotherapy considerably improves the effectiveness of manual lymphatic drainage (MLD) in patients with lipedema: A two-armed, randomized, controlled pragmatic trial [moderate evidence] ↩
Journal of Wound Care 2020: Lipoedema: a paradigm shift and consensus [expert review; ungraded] ↩
Archives of Plastic Surgery 2017: Liposuction in the treatment of lipedema: A longitudinal study [case-control study; weak evidence]
Dermatologic Surgery 2020: Prevention of progression of lipedema with liposuction using tumescent local anesthesia: Results of an international consensus conference [expert consensus; ungraded]
Dermatologic Therapy 2019: Treatment of lipedema by low-volume micro-cannular liposuction in tumescent anesthesia: Results in 111 patients [case-control study; weak evidence] ↩